J Thromb Heamost:口服避孕药、血栓与静脉血栓栓塞的风险:系统回顾和荟萃分析
2016-07-06 Seven L 译 MedSci原创
根据一项荟萃分析的结果,严重的遗传性易栓症女性使用口服避孕药会增加静脉血栓栓塞(VTE)的风险。格罗宁根大学医学中心的Elizabeth F.W. van Vlijmen博士和他的同事利用MEDLINE和EMBASE数据库,对12项病例对照研究和3项队列研究的数据进行了分析,评估家庭中有轻度和重度的遗传性易栓症妇女使用复方口服避孕药后的首次VTE的额外风险。研究人员定义为轻度血栓形成倾向为因子V
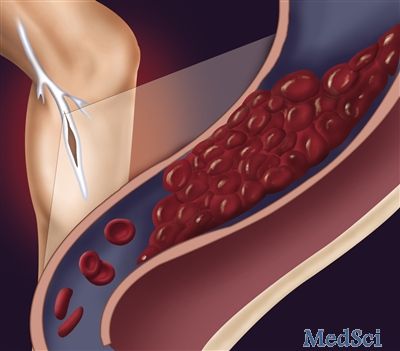
根据一项荟萃分析的结果,严重的遗传性易栓症女性使用口服避孕药会增加静脉血栓栓塞(VTE)的风险。
格罗宁根大学医学中心的Elizabeth F.W. van Vlijmen博士和他的同事利用MEDLINE和EMBASE数据库,对12项病例对照研究和3项队列研究的数据进行了分析,评估家庭中有轻度和重度的遗传性易栓症妇女使用复方口服避孕药后的首次VTE的额外风险。
研究人员定义为轻度血栓形成倾向为因子V Leiden和凝血酶原基因G20210A突变。定义严重的血栓形成倾向为抗凝血酶缺乏、蛋白C缺乏、蛋白S缺乏、双杂合子或莱顿和因子V Leiden和凝血酶原基因G20210A突变纯合子。
使用口服避孕药增加轻度和重度血栓形成倾向妇女VTE风险(轻度:RR = 5.89; 95% CI, 4.21-8.23;重度:RR = 7.15; 95% CI, 2.93-17.45)。
家庭的队列研究表明,100丸年随访中的绝对VTE风险在重度栓形成倾向女性中更大(重度:ORs = 4.3 to 4.6;轻度:ORs = 0.49 to 2)。
研究人员还指出,无血栓形成倾向的女性使用口服避孕药后,其VTE风险也会增加。但是研究人员指出,这一群体包括家庭成员有血栓形成倾向的家族史。
家族队列研究中,没有因子V Leiden或凝血酶原基因G20210A突变的女性,使用口服避孕药后的VTE发生率从0 (95% CI, 0-5.5)到0.19 (95% CI, 0.07-0.41)。
非双杂合子或FV Leiden 或凝血酶原基因G20210A突变纯合子女性的VTE发生率(每100丸年)为0.19 (95% CI, 0.07-0.42)。没有抗凝血酶、蛋白C或蛋白S缺乏的女性其VTE发生率从0.48 (95% CI, 0.01-1.4)到0.7 (95% CI, 0-3.7)。
根据此研究,对于有血栓形成倾向的女性而言,避孕方法的选择上应仔细询问医生,使她们能够做出最佳避孕选择。
原始出处:
an Vlijmen EF, et al. Combined oral contraceptives, thrombophilia and the risk of venous thromboembolism: a systematic review and meta-analysis.J Thromb Heamost. 2016;doi:10.1111/jth.13349.
Combined oral contraceptives increase risk for VTE in women with severe thrombophilia.Healio.July 5, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#静脉血#
23
#荟萃#
21
#静脉#
22
#荟萃分析#
31
谢谢分享学习
68
谢谢谢谢分享
55
#系统回顾#
33
#口服避孕药#
23