Cancer Cell:高通量肿瘤功能基因组注释与分析
2018-03-25 BioArt BioArt
人类在征服疾病的进程中虽然曲折前行,但是收获匪浅。基于癌症的诊断与治疗,已经由传统的化疗、放疗逐渐发展为靶向疗法、免疫疗法,并继续走向组合疗法和精准个体医疗。癌症,和其他很多复杂综合症一样,在病人群体中存在着极大的基因型(genotype)差异,导致很难用单一的药物控制症状。随着新一代测序技术的建立和测序成本的大幅度降低,越来越多的病人可以完成全基因组测序(whole-genome sequenc
正是在这个背景下,University of Texas MD Anderson Cancer Center的Han Liang(梁晗)、 Song Stephen Yi(伊松。BioArt注: 伊松老师最近转到了UT Austin,但是仍然是MD Anderson 的adjunct professor)、 Nidhi Sahni和Gordon Mills四个团队的科研人员,合作建立了一套高通量的功能筛选系统,成功地解析了人类多种癌症中常见的基因点突变和基因融合的生物学功能,绘制了蛋白质组水平的变异功能图谱,揭示了不同基因型(genotype)和表型(phenotype)之间的复杂关系。
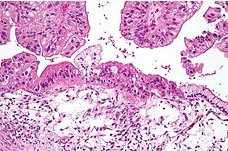
据BioArt了解,这项工作前后花了好几年的时间。研究人员系统地探索了上千种不同的基因突变(包括基因扩增、点突变、插入和缺失、基因融合等)在多种癌症中的功能,利用半定量的肿瘤细胞健康模型(tumour-fitness model),先将不同的癌症相关基因划分为激活型、抑制型和非功能型。在此基础上,再将特异性的基因突变与相关的野生型基因进行同等条件比较,再划分为“去激活型”、“更激活型”、“去抑制型”、“更抑制型”等多种细致的类别。为了保证结果的可靠性,研究人员使用了完全独立的另外一种细胞株进行验证。在多数情况下,实验揭示的肿瘤基因突变功能得到了验证。该成果与以往基于基因水平的研究相比,大大提高了系统生物学高通量解析基因组变异的效率和分辨率,为个体化医疗和检测奠定了坚实的基础。
在最近的一段时间里,Harvard Medical School、Broad Institute等科研机构也开展了一些相关的攻克基因突变功能的实验工作。这些工作采用各自独特的筛选平台,均发现同一基因里的不同变异往往展示截然不同的生物学功能。这些结果往往得到基因转录组或蛋白组数据的进一步支持验证。
总体而言,基因内部突变特异性的功能向传统生物学提出挑战,以基因为单位的研究不足以解释基因潜在的所有功能。重要的是,这些成果为癌症个体化精准医疗和预防检测带来了福音。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#cancer cell#
37
#高通量#
29
#CEL#
35
#Cell#
35
学习谢谢分享
43