PNAS:科学家阐明细菌性腹泻的发病机理
2016-07-07 佚名 生物谷
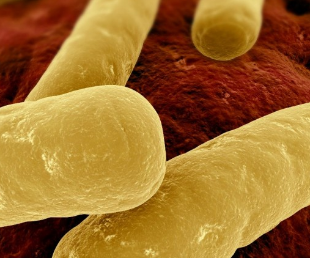
抗生素的摄入通常会损伤肠道的天然菌群,从而就会抑制机体控制病原体的能力,进而引发常见的腹泻和肠道炎症等病症,艰难梭菌(Clostridium difficile)就是一种通过毒素攻击肠道细胞的病原体,其会在肠道细胞表面形成一种特殊的突起结构,进而使得更多细菌在肠道细胞表面着陆引发感染。近日,来自弗莱堡大学的研究人员通过研究揭示了艰难梭菌的毒素CDT形成这些细胞突起的分子机制,相关研究刊登于国际杂志
抗生素的摄入通常会损伤肠道的天然菌群,从而就会抑制机体控制病原体的能力,进而引发常见的腹泻和肠道炎症等病症,艰难梭菌(Clostridium difficile)就是一种通过毒素攻击肠道细胞的病原体,其会在肠道细胞表面形成一种特殊的突起结构,进而使得更多细菌在肠道细胞表面着陆引发感染。近日,来自弗莱堡大学的研究人员通过研究揭示了艰难梭菌的毒素CDT形成这些细胞突起的分子机制,相关研究刊登于国际杂志PNAS上,通过研究CDT毒素,研究者们就可以更好地理解病原体诱发肠道炎症的分子机制,这样科学家们就能够利用毒素作为工具来阐明疾病发生背后的分子机理。
艰难梭菌会产生毒素来破坏肠道细胞结构,而这就会抑制肠道细胞间的接触从而造成功能性障碍,进而引发腹泻和炎症发生;细胞结构的两个重要元件是肌动蛋白和微管,其在维持细胞结构、功能屏障以及细胞运动过程中扮演着重要的作用,而艰难梭菌产生的CDT毒素就会修饰肌动蛋白,从而阻断其结构链的形成并且干扰正常功能,其中一个重要的结果就是导致微管链的形成更加容易,并且增加到一定程度从而导致许多细胞前突出现,而这最终就会形成一种肠道细胞表面网络结构,促进细菌与宿主细胞的接触。
然而CDT毒素如何形成这些细胞突起目前研究者并不清楚,文章中,研究者发现,毒素影响肌动蛋白和微管蛋白之间的协调作用还需要第三种元件:隔膜蛋白(septins),在人类细胞中有多达13种隔膜蛋白,其可以彼此接触形成链状、环状结构,而这一过程称之为聚合作用;CDT就可以以这种方式来修饰肌动蛋白从而使得隔膜蛋白不能够结合到肌动蛋白上,相反其会迁移到细胞膜上形成套环样的隔膜蛋白聚合体,隔膜蛋白可以直接同生长中的微管的末端直接接触,并且作为向导来指导微管生长。
本文研究为后期科学家们深入理解隔膜蛋白套环结构的形成提供了新的线索,Cdc42和Borg蛋白可以调节隔膜蛋白向细胞膜的转运,而这对于套环结构的形成非常关键,同时隔膜蛋白因可以形成神经突起,在人类神经系统中扮演着重要作用。最后研究者表示,肌动蛋白、微管蛋白及隔膜蛋白三者可以相互作用形成微观结构,后期研究者还将继续对CDT毒素进行深入研究帮助更好地理解人类疾病疾病的发病过程。
原始出处
Thilo Nölke, Carsten Schwan, Friederike Lehmann, Kristine Østevold, Olivier Pertz, Klaus Aktories.Septins guide microtubule protrusions induced by actin-depolymerizing toxins likeClostridium difficiletransferase (CDT)y.PNAS.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







原文怎么找啊
25
#发病机理#
35
#PNAS#
18
研究很创新,值得学习
34
梭菌研究,细菌与肠道互作,很不错的ideal
63