食管癌质子治疗最新回顾性研究,用实际数据给出推荐食管癌选择质子治疗的答案!
2022-09-07 厚朴方舟 厚朴方舟
目前局限性食管癌治疗的金标准仍然是手术,但是一些患者确诊时,由于肿瘤已经进展到晚期、身体情况不佳、不愿意接受手术等等原因无法手术,同步放化疗成为这些患者的主要选择。
2021年8月,日本筑波大学附属医院发表在《Journal of Personalized Medicine》的一篇述评回顾,从日本质子、碳离子等粒子治疗的基础和临床应用综合探讨日本粒子治疗在多学科治疗中的作用,其中,对质子治疗食管癌的效果进行了详细回顾。
为什么推荐食管癌患者选择质子治疗?
文章中指出,目前局限性食管癌治疗的金标准仍然是手术,但是一些患者确诊时,由于肿瘤已经进展到晚期、身体情况不佳、不愿意接受手术等等原因无法手术,同步放化疗成为这些患者的主要选择。
但是,研究证实使用光子放疗与食管癌患者出现心肺毒性和晚期不良反应有关,而且食管癌患者出现的心肺毒性会影响食管癌治疗中胸部高剂量放射的管理。同时,食管癌同步放化疗后可能出现局部复发和区域复发。因此在避免心脏、肺部放射剂量的同时增加靶区剂量是改善食管癌治疗结果的合理方法。
简单来说,就是光子放疗的剂量较高会导致食管周围器官或组织,如心脏、肺部等出现严重的并发症,比如食管穿孔、放射性食管炎、食管梗阻、气道反应、放射性肺炎、心脏损伤和全身症状等,严重的甚至会危及患者的生命安全。但是降低光子放疗的剂量会导致食管癌的复发率增加。
因此,质子治疗凭借特殊的“布拉格峰效应”,为食管癌的治疗提供了便利。与光子放疗相比,质子治疗可以减少心肺等风险器官的辐射剂量,降低并发症,同时无需降低针对肿瘤的辐射剂量,提高食管癌的治愈率。
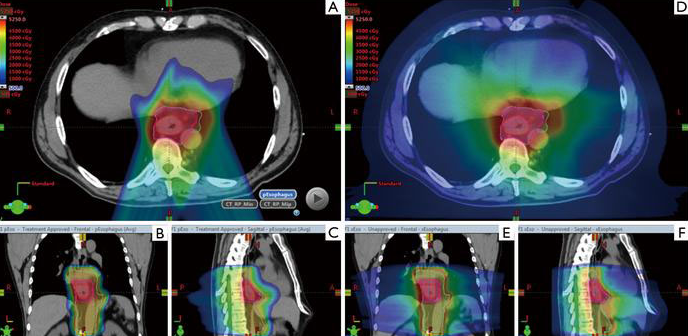
▲质子治疗食管癌,
质子治疗食管癌的有效性与安全性
01
2015年的一项研究评估了不可切除食管癌患者采用质子治疗联合化疗的效果。研究纳入了2008 年至 2012 年确诊的40名食管癌患者,采用顺铂、5氟尿嘧啶联合中位剂量为60 Gy (RBE)的质子治疗进行治疗。
研究结果显示,采用质子治疗联合化疗的2年疾病特异性生存率为77%,2年局部控制率为66%,并未出现 3 级或以上的心肺毒性。研究证实,通过质子联合化疗治疗食管癌是可行的。
 02
02
2019年一项日本多中心回顾性研究评估了质子治疗食管癌的效果。该研究纳入了2009年至2013年在日本四个机构接受治疗的202例食管癌患者(195例鳞状细胞癌和7例腺癌)。
研究结果显示,质子治疗Ⅰ-Ⅱ期食管癌患者的5年总生存率(OS)为75.4%,5年局部控制率为74.0%;Ⅲ-Ⅳ期食管癌患者的5年OS为36.8%,5年局部控制率为53.8%。此外,仅在1.5%(3名)食管癌患者中观察到3级心肺毒性。
该研究证实,与光子放疗相比,质子治疗食管癌的效果并不逊色,且毒性发生率较低,可以作为食管癌的替代疗法。

▲质子治疗食管癌的5年生存率,
03
2020年的一项随机研究比较了调强放疗(IMRT)和质子治疗的总毒性负担(TTB)和生存期。研究共纳入了 145 名食管癌患者(72 名患者接受IMRT治疗,73 名接受质子治疗)。
注:总毒性负担(TTB) 定义为≥ 2 级肺炎、心脏或食管毒性
研究结果显示,质子治疗食管癌可以在保证效果的同时,降低总毒性负担即心肺毒性和术后并发症较少。具体数据为,调强放疗(IMRT)后的平均总毒性负担是质子治疗的2.3倍(39.9 vs 17.4);调强放疗(IMRT)的平均术后并发症 (POC)分数比质子治疗高出7.6倍(19.1 vs 2.5);并且两者的3年总生存率相似(44.5% v 44.5%)。

▲IMRT与质子治疗食管癌的生存期对比

▲IMRT与质子治疗食管癌的总毒性负担对比,
除了以上三项研究之外,还有许多研究证实了质子治疗食管癌的显著效果:

▲光子放疗与质子治疗食管癌的安全性对比研究
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#最新#
43
值得学习
34
#质子治疗#
0
#食管#
53
#回顾性研究#
43