Mol Syst Biol:PDK4可作前列腺癌的独立预后标志物
2020-04-26 竹子 转化医学网
前列腺癌(PCa)是全世界男性中第二常见的癌症,也是第五大死于癌症的主要原因。
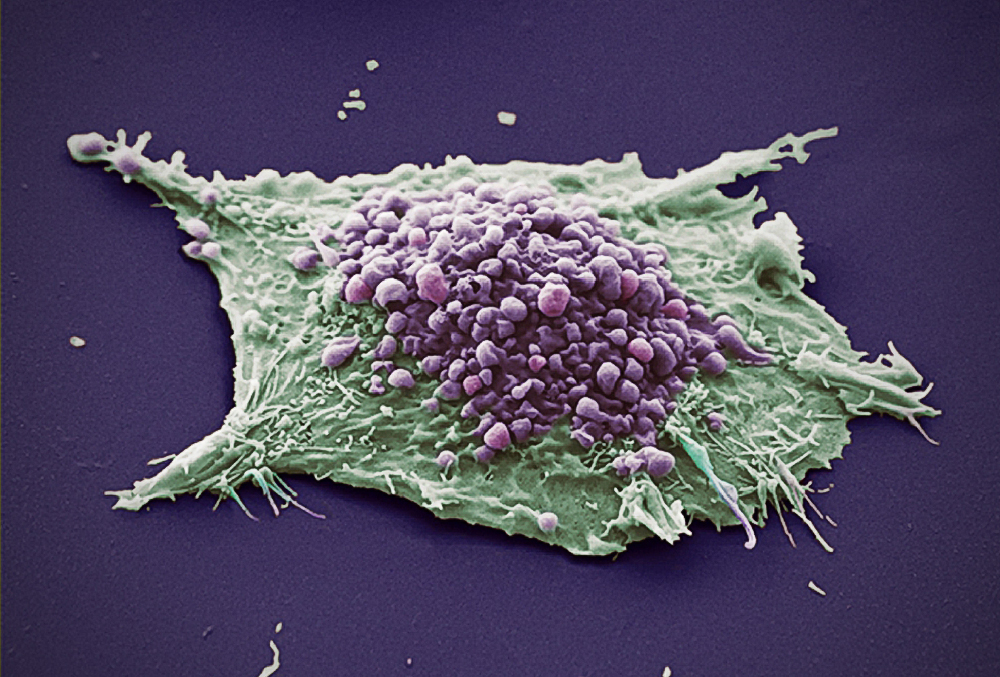
前列腺癌(PCa)是全世界男性中第二常见的癌症,也是第五大死于癌症的主要原因。PCa具有广泛的临床表现,因此迫切需要生物标志物来进行风险分层。如今,研究人员通过利用转录组学数据的基因共表达网络,以及从人和鼠前列腺石蜡包埋组织(FFPE)样品中提取的激光显微切割的蛋白质组学,找到了潜在的风险分层生物标志物。
统计数据表明,奥地利每年约有5,600名男性被诊断出患有前列腺癌,这意味着它约占男性所有癌症的四分之一。对于某些人来说,癌症发展缓慢并且需要最少的治疗,但是其他人则具有侵略性的疾病形式,并且进展很快。为了能够更有效地治疗前列腺癌,需要更好地理解在肿瘤分子水平上发生的复杂机制。在2015年,由维也纳医科大学的分子病理学家卢卡斯·肯纳(Lukas Kenner)领导的团队意外发现了STAT3蛋白在小鼠模型中在前列腺癌中起着抑癌作用。他们表明,与高水平的患者相比,癌细胞中STAT3水平低的患者的疾病进展显着恶化。
基于以前研究的发现,最近由维也纳医科大学病理学系肯纳团队的博士候选人莫妮卡·奥伯哈伯(Monika Oberhuber )与奥地利生物技术研究医学中心,COMET能力中心(由奥地利研究促进局(FFG)资助)共同进行了一项研究。研究发现,丙酮酸脱氢酶激酶4(PDK4)与STAT3蛋白有直接相关性,可将其基因表达作为前列腺癌的独立预后标志物,可预测前列腺癌复发与诊断风险因素。该研究发表在《分子系统生物学》期刊上。
该研究分析了许多大型患者数据集,并比较了组织中STAT3高表达和低表达的患者。这导致鉴定不同基因簇的表达特征之间的相关性。研究人员发现,STAT3低的患者的代谢活跃。代谢(尤其是细胞呼吸)在前列腺肿瘤中的活性比在健康前列腺组织中的活性高得多。这为肿瘤提供了额外的生长能量。STAT3低的患者表现出更高的细胞呼吸作用和更活跃的肿瘤,其中形成了许多新蛋白质。
奥伯哈伯还用石蜡包埋组织切片研究了低STAT3与活性代谢之间的关系。用激光显微镜将肿瘤组织与健康组织分离,然后使用质谱分析。
有趣的是,结果显示STAT3和PDK4之间存在直接相关性,从而减慢了细胞呼吸。显示STAT3低的患者也具有低PDK4,这可以证明PDK4直接受STAT3调节。这意味着PDK4水平可以很好地预测疾病的进程。换句话说,PDK4低的前列腺癌患者的预后要比PDK4高的前列腺癌患者差。PDK4基因在其他肿瘤和疾病(例如糖尿病)的发生中也起着重要作用。现在计划对PDK4进行后续研究,以研究其在前列腺癌治疗中的潜在应用。
原始出处:Monika Oberhuber, Matteo Pecoraro, Mate Rusz et al. STAT 3 ‐dependent analysis reveals PDK 4 as independent predictor of recurrence in prostate cancer. Molecular Systems Biology (2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#预后标志#
35
#标志物#
32
#Biol#
32
#PDK4#
24
#Bio#
22
#预后标志物#
0
前列腺癌相关研究,学习了,谢谢梅斯
32