Clin Oral Investig:口腔癌放疗会影响釉质的显微硬度以及相关联的缩进形态
2017-11-25 lishiting MedSci原创
这篇研究的目的是为了在体内体外评估高剂量的放射线疗法对釉质的显微硬度和相关联的缩进模式形态的影响。
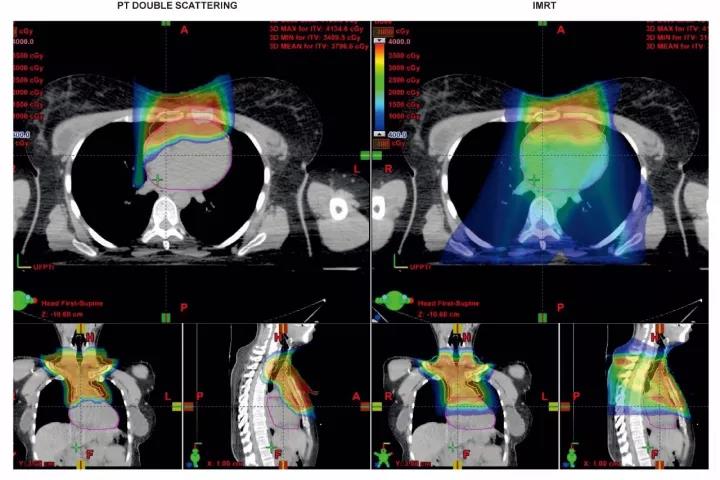
这篇研究的目的是为了在体内体外评估高剂量的放射线疗法对釉质的显微硬度和相关联的缩进模式形态的影响。研究通过3个实验组评估釉质内层、中间层和外层的显微硬度:对照组(未放疗);体外辐照;体内辐照。体外样本暴露于模拟放疗中,体内样本为口腔癌患者放疗过后拔除的牙齿。通过SEM影像分析缩进模式以计算显微硬度值,并且在放疗前后评估釉质的机械形态特质。结果显示,与对照组相比,釉质中间层和外层区域的显微硬度在体内体外辐照后均表现出明显的减弱(p<0.05)。研究观察到2种缩进模式:模式A-围绕缩进边缘存在微裂纹,代表着局部形变能量的分散;模式B-洁净、尖锐的缩进边缘。与对照组相比,釉质所有区域的洁净微缩进模式百分比在体内体外辐照后均明显升高。洁净微缩进的最高百分率(65%)发生在体内辐照组的釉质靠近釉牙本质界的内侧区域。结论:这篇研究是第一次发现体内外的辐照会改变釉质的显微硬度。同样,缩进模式的差异也表明,体内体外辐照可能会使釉质变的更加脆弱。临床意义:釉质辐照后机械形态特质的改变可能是导致口腔癌放疗后病理性釉质脱层的一个原因。原始出处:Seyedmahmoud R, Wang Y, et al
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#显微硬度#
41
#Oral#
28
#EST#
32
学习了.谢谢
81
不错的文章值得推荐
67