Neuroradiology:伴发的静脉畸形在海绵状血管瘤破裂中的作用
2020-03-16 杨中华 脑血管病及重症文献导读
2020年1月来自北京天坛医院的Shuo Zhang等在Neuroradiology上公布了他们的研究结果,目的在于寻找 CCM-DVA 密切相关的危险因素,为制定合理的个体化治疗方案奠定基础。
脑海绵状血管畸形(Cerebral cavernous malformation,CCM)是一种常见的脑血管畸形,人群尸体解剖的研究中 CCM 的发生率为0.5%,占血管畸形患者的5-13%。CCM 最常见于慕上,反复颅内出血是主要表现。未破裂 CCM 的平均出血率为每年0.4-0.6%,破裂 CCM 的再出血率明显升高,大约为每年4.5-22.9%。与其他形式的脑血管畸形比如动静脉畸形和 CCM,发育性静脉畸形(developmental venous anomaly,DVA)的发病率更高,为3%。有人认为的自然史是良性的,大部分患者没有症状,出血发生率低至每年0.22-0.68%,但是当伴发其他颅内血管畸形时比如 CCM,DVA 常常会加速它们的进展。
CCM 伴 DVA(CCM-DVA)被认为是最常见的颅内血管畸形类型,首次由 Roberson 于1974年报道,1984年 McCormick 对其进行了分类。大约8-33%的 DVA 和 CCM 是伴发的,散发 CCM-DVA 比家族者更常见。以前对 CCM 破裂因素的研究发现,女性、年轻、幕下病灶、eloquent location以及合并 DVA 与较高的出血风险有关。
因为相当大一部分 CCM 伴发 DVA,从血流动力学角度来看不同位置结构的关系会影响到病灶的破裂。在以前的研究中,伴发 DVA 往往作为 CCM 破裂的潜在危险因素进行讨论,但是 没有对 CCM 合并 DVA的患者群体进行过大规模研究,很少有研究将二者的关系作为发生出血的指标。考虑到这些因素,我们决定根据以前研究中讨论的危险因素来探讨成人 CCM-DVA 的关系,包括 CCM-DVA 的数量和结构特征,主要是希望在涵盖最全面的影响因素的前提下预测出血的风险,并为将来的临床决策提供证据。
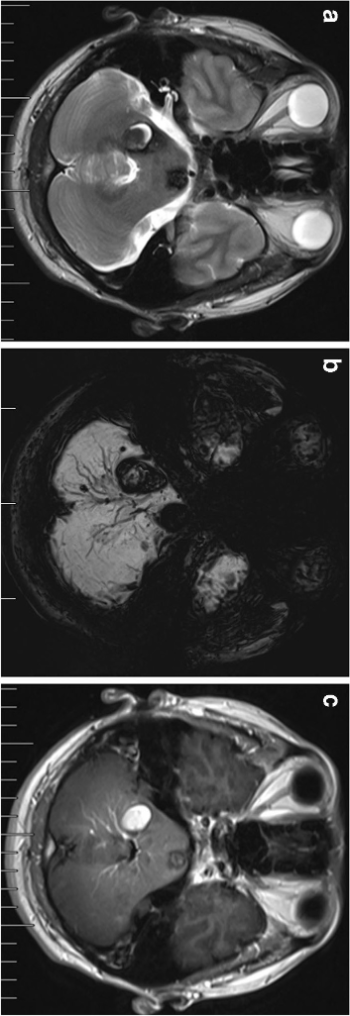
示例:多发 CCM-DVA 患者,右侧小脑 CCM 以及临近的 DVA。T2WII 未见 DVA(a 图),但是 SWI(b 图)和 T1增强(c 图)可见 DVA。在 SWI 上(b 图)可见DVA 远端分支多处微出血,高度怀疑 CCM,但是增强扫描未发现这些微出血:
2020年1月来自北京天坛医院的Shuo Zhang等在Neuroradiology上公布了他们的研究结果,目的在于寻找 CCM-DVA 密切相关的危险因素,为制定合理的个体化治疗方案奠定基础。
在这个回顾性研究中,纳入了2014-2017年研究者所在医院的 CCM-DVA 门诊患者,并且进行过 SWI 和增强 MRI 扫描。CCM-DVA 病灶按照部位和 CCM 与 DVA之间的定量关系分为三型。
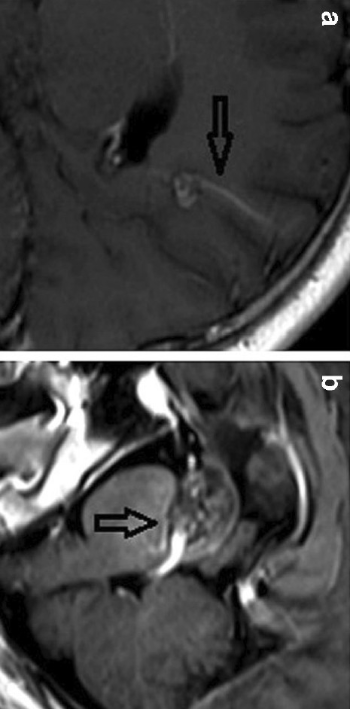
示例:CCM-DVA 关系的不同分类。a(I 型),CCM 位于枕叶,单个引流静脉到皮层。b 和 c(II 型),CCM 位于 DVA 干部(trunk),被多支静脉引流围绕。d(III 型),DVA 由多个迂曲的引流静脉组成,最后汇集成一个集合静脉,CCM 位于DVA远端分支的转折点上,多支引流静脉最后汇合成集合静脉:
总共319例成人患者,平均年龄41.2+-11.9岁,单变量和多参数回归分析发现破裂更加常见于:以前出血,III 型 CCM-DVA,病灶体积>1cm3,幕下病灶特别是位于中脑,桥脑,延髓。Caplan-Meier曲线显示 III 型 CCM-DVA 病灶、功能区病灶、病灶体积>1cm3以及幕下病灶者无出血生存率更低。
最终作者认为 CCM 和 DVA 关系的分类预测破裂风险是有意义的,位于 DVA 远端分支的 CCM 破裂风险更高。
原始出处:Shuo Zhang, Li Ma, Chunxue Wu, et al. A rupture risk analysis of cerebral cavernous malformation associated with developmental venous anomaly using susceptibility-weighted imaging. Neuroradiology. 2019 Sep 3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
0
#血管瘤#
43
#畸形#
38
#海绵状血管瘤#
37
#海绵状#
39