快速处理应激性溃疡“大出血”
2016-09-11 Tony Ge 医学界急诊与重症频道
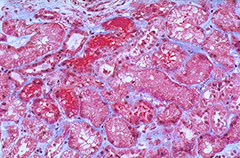
应激性溃疡概念:应激因素如严重创伤,周身感染,严重烧伤,休克、MODS等导致严重应激反应情况下,胃粘膜出现急性炎症、糜烂或溃疡后引起消化道大出血或胃穿孔。易引起应激性溃疡的的急诊科高危因素有哪些?① 65 岁以上高龄;② 严重创伤包括如颅脑外伤、烧伤、胸、腹部复杂,困难大手术等;③ 合并休克或持续低血压;④ 严重全身感染;⑤ 并发多脏器衰竭、机械通气 3 天以上;⑥ 重度黄疸;⑦ 合并凝血机制障碍
易引起应激性溃疡的的急诊科高危因素有哪些?
① 65 岁以上高龄;
② 严重创伤包括如颅脑外伤、烧伤、胸、腹部复杂,困难大手术等;
③ 合并休克或持续低血压;
④ 严重全身感染;
⑤ 并发多脏器衰竭、机械通气 3 天以上;

⑥ 重度黄疸;
⑦ 合并凝血机制障碍;
⑧ 脏器移植术后;
⑨ 长期应用免疫抑制剂与胃肠道外营养;
⑩ 1 年内有消化道溃疡病史。
预防措施
1. 针对应激性溃疡的高危患者进行严密的胃肠监护及预防措施。
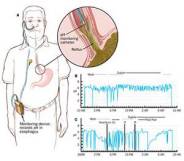
2. 定期定时检测胃液 pH 或作 24h 胃 pH 检测,并定期检测粪便隐血,重大手术病人需明确有否合并溃疡。
3. 治疗原发病,消除应激因素,维护组织的灌注和氧供,防治组织低氧。
预防应激性溃疡的常用药物
1. 抑酸药:质子泵阻滞剂(PPI)奥美拉唑、组胺受体阻滞剂法莫替丁、雷尼替丁、西咪替丁等保持胃内 pH > 4 。
2. 胃管内注入抗酸药氢氧化铝、铝碳酸镁、5%碳酸氢钠溶液等,使胃内 pH ≥ 4。
3. 硫糖铝、前列腺素E 等保护胃粘膜剂。
4. 支持疗法如早期恢复肠内营养,早期进食,以中和胃酸,增强胃肠粘膜屏障功能。
5. 补充与调整低蛋白血症、纠正电解质和酸硷平衡紊乱。

应激性溃疡并发消化道大出血的救治要点
1. 快速补液及输血,稳定血液容量及循环。
2. 快速提高胃内 pH ≥ 6。可选用奥美拉唑针剂,H2 阻滞剂针剂。
3. 胃内灌注碱性药物(如氢氧化铝等),使胃液 pH 在 6 以上。
4. 必要时选用生长抑素类药物。
5. 强化粘膜保护剂和抗生素的应用,以防止烧伤患者合并菌群移位。

6. 输注新鲜血小板悬液、凝血酶原复合物、促进凝血的药物有助于合并有凝血机制障碍的患者止血。
7. 紧急胃镜及内镜下作止血治疗。
8. 经药物和内镜介入治疗止血无效者可以考虑外科手术治疗。
9. 在出血停止后,继续使用 PPI、H2 阻滞剂等药物 4~6 周,至溃疡愈合。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








很好的诊疗规范,学习了
28
学习了,赞一个!!!
33
学习了,赞一个!!!
27
学习了,赞一个!!!
36
#大出血#
19
#应激#
16
#应激性溃疡#
28
学习了,赞一个!!!
49