为什么叫半卵圆中心?
答:半卵圆中心是一个形态学名词,为一区域白质的统称,具体位置为胼胝体(相当于侧脑室体部上方)上部层面的大脑白质。因在横切面上,左右两侧合起来呈卵圆形,而单侧为半卵圆形,故称为半卵圆中心。其包含投射、联络及连结三种纤维。

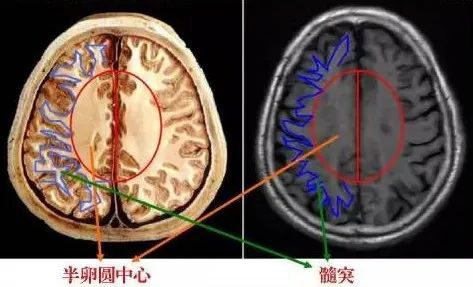
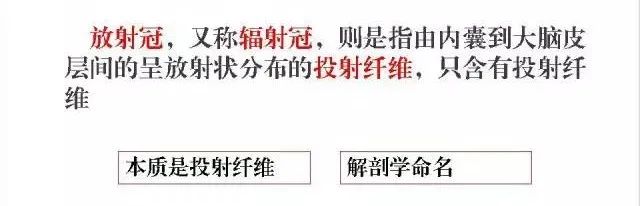
半卵圆中心此断面恰经胼胝体上方,可见大脑半球的髓质形成半卵圆中心。此处大脑半球的髓质成自三种纤维:
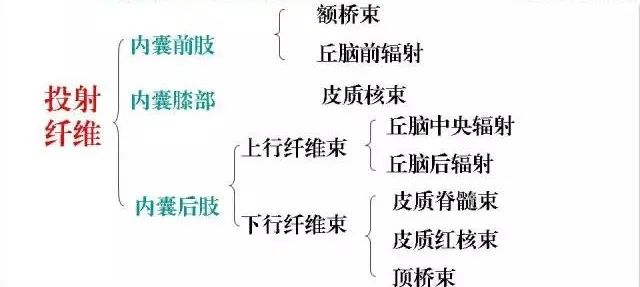
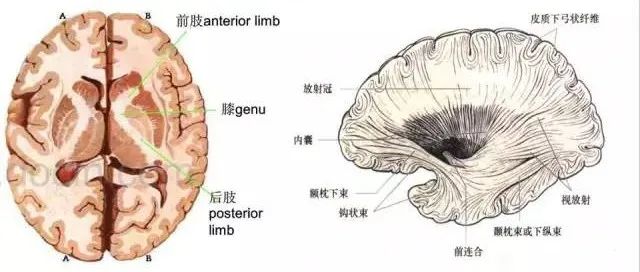
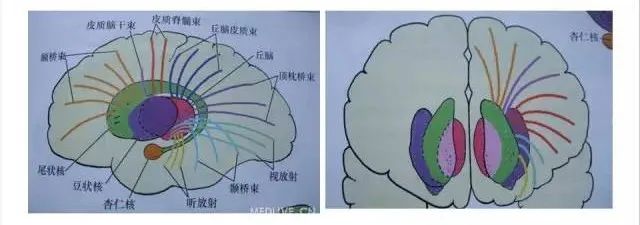
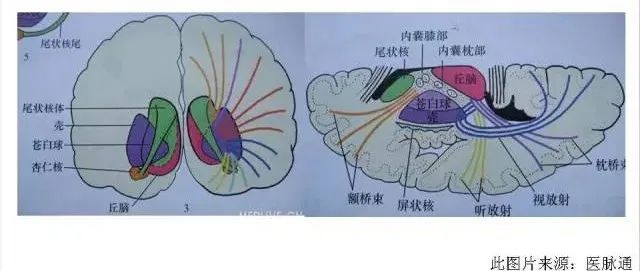
①投射纤维:连接大脑皮质和皮质下诸结构,呈扇形放射,称辐射冠;
②联络纤维:连接本侧半球各皮质,人脑的联络纤维极为发达,与投射纤维和连合纤维相比,其数量最大;
③连合纤维:连接左、右大脑半球的相应皮质区。
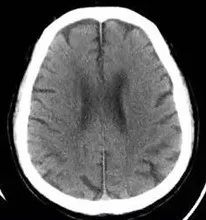
半卵圆中心的纤维主要为有髓纤维,故在MRI T1加权像上呈高信号,在CT图像上为低密度。脑内的脱髓鞘病变如多发性硬化、肾上腺脑白质营养不良以及脑结节硬化症等,常于该区出现单发或多发病灶。
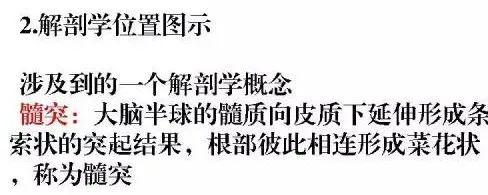
放射冠(辐射冠)
什么是放射冠?
放射冠是指由内囊到大脑皮层间的放射状纤维白质,呈放射状分布的投射纤维,只含有投射纤维到皮质(放射冠部分纤维会穿过半卵圆中心,或者说沿途成为半卵圆中心的一部分)。
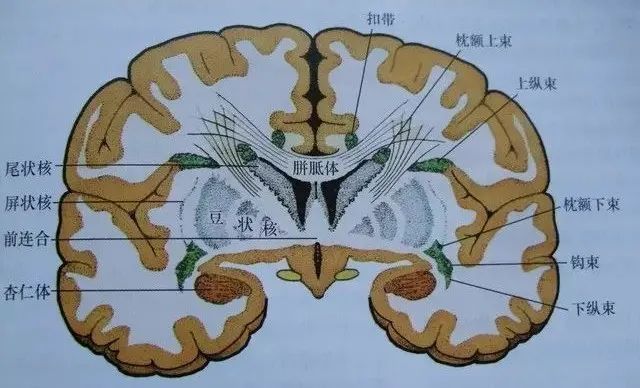
二者的关系
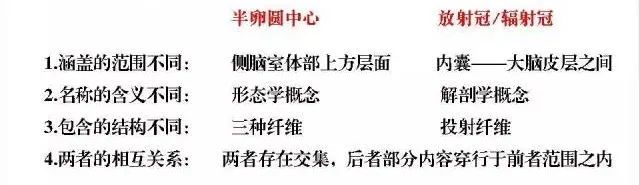
半卵圆中心

放射冠
一般半卵圆中心是指脑室上部的脑白质区域(层面上不出现侧脑室),而放射冠是指两侧侧脑室周围的脑白质层面。
可以这样来简单理解:
放射冠范围较半卵圆中心要大,半卵圆中心通常指的是侧脑室顶部以上的白质区,即是说看到半卵圆中心的时候已经看不到侧脑室。
书写报告时可以这样来定位:
在侧脑室顶部以上者称之为左侧/右侧半卵圆中心,还能看到侧脑室的情况下用侧脑室前角旁/后角旁/体旁来定位即可。当然,基底节区和丘脑要另当别论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







通俗易懂,解决了心中疑惑
41
非常好 终于理解啦
40
谢谢分享
0
谢谢分享
46