Nature子刊:小分子治疗3型乌谢尔综合征听觉丧失
2016-05-07 MedSci MedSci原创
乌谢尔综合征(Usher syndrome,USH)是一种遗传性疾病,显著特点是先天弱听或耳聋,以及进行性的视觉丧失。临床上依据相关的基因不同,将乌谢尔综合症分为三种不同的亚型。3型乌谢尔综合症由编码CLRN1(clarin-1 protein)的基因发生突变导致,患者出生时一般听力正常,随后的几十年会出现进行性视觉和听觉丧失,并伴有平衡障碍。这种疾病目前还没有有效的治疗方案,可以说是某种程度上的
乌谢尔综合征(Usher syndrome,USH)是一种遗传性疾病,显著特点是先天弱听或耳聋,以及进行性的视觉丧失。临床上依据相关的基因不同,将乌谢尔综合症分为三种不同的亚型。3型乌谢尔综合症由编码CLRN1(clarin-1 protein)的基因发生突变导致,患者出生时一般听力正常,随后的几十年会出现进行性视觉和听觉丧失,并伴有平衡障碍。这种疾病目前还没有有效的治疗方案,可以说是某种程度上的“无药可治”。
最近发表在Nature Chemical Biology上的一项最新研究报道了首个治疗3型乌谢尔综合症模式小鼠进行性听觉丧失的小分子药物。该靶向治疗方法的发现为成千上万3型乌谢尔综合症患者及他们的家庭带来了希望。这项研究由凯斯西储大学医学院的Kumar N. Alagramam博士和Yoshikazu Imanishi博士领导,他们发展了一种小分子BF844(见下图)可以抑制3型乌谢尔综合症常见的突变基因CLRN1N48K(Clarin-1-N48K)的表达。(A small molecule mitigates hearing loss in a mouse model of Usher syndrome III. Nat. Chem. Biol., DOI: 10.1038/nchembio.2069)

该团队使用了一种独特的研究策略,包括基于细胞的高通量筛选,从50000个分子中找出稳定突变基因CLRN1N48K效果最好的320个分子;第二次筛选排除一些酶的抑制剂(减少药物的副作用)、产生荧光的分子以及不太稳定的分子;最后是反复优化分子的构效关系,最终找到最佳分子BF844。
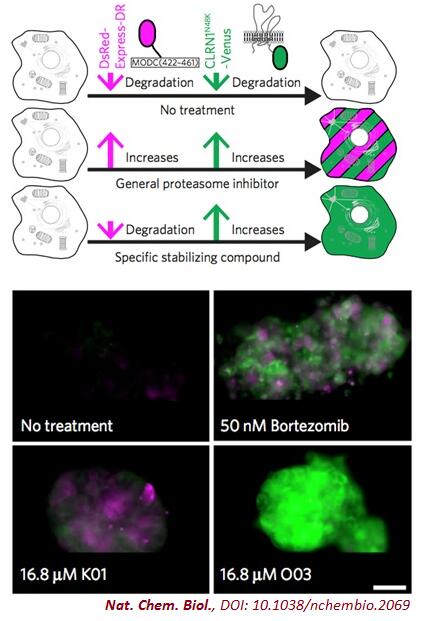
研究者建立一中双报告系统筛选潜在的小分子。当分子无效时细胞不显色;当分子既能稳定CLRN1N48K,又表现出对酶的抑制作用时,细胞显红绿混合的荧光;只有当分子仅稳定CLRN1N48K,而不抑制酶时,细胞显绿色荧光。图片来源:NPG
为了测试BF844的效果,医学院的科学家发展了一种模拟3型乌谢尔综合症进行性听力丧失的模式小鼠,结果表明BF844能有效减缓听力衰退的进程,并防止耳聋。

Kumar N. Alagramam博士(左)和Yoshikazu Imanishi博士(右)。图片来源:Case Western Reserve University
Alagramam盛赞这一治疗方案非常具有应用潜力,因为它能在病人出现听力衰退症状之前先发制人。

Imanishi则认为这项成果的意义不仅仅在于3型乌谢尔综合症和听力衰退,由于CLRN1N48K还与视觉丧失有关,该小分子理论上还能阻止患者的失明。另外,许多单基因失调是由使蛋白产物不稳定的点突变导致,他们的药物研发策略理论上可以用于寻找所有稳定这些突变基因蛋白的药物。
令人感慨的是,资助这项研究的Cindy Elden女士就是3型乌谢尔综合症患者,她30岁之前一直被误诊为2型乌谢尔综合症,Elden的父亲为了治疗女儿的疾病奔波了很长时间。因此他们成立了3型乌谢尔综合症基金,呼吁人们更加关注这一基因疾病,并资助针对该疾病的基础和临床研究。
原始出处:
Alagramam KN, Gopal SR, Geng R, Chen DH, Nemet I, Lee R, Tian G, Miyagi M, Malagu KF, Lock CJ, Esmieu WR, Owens AP, Lindsay NA, Ouwehand K, Albertus F, Fischer DF, Bürli RW, MacLeod AM, Harte WE, Palczewski K, Imanishi Y.A small molecule mitigates hearing loss in a mouse model of Usher syndrome III. Nat Chem Biol. 2016 Apr 25. doi: 10.1038/nchembio.2069
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Nat#
30
#小分子#
31
#综合征#
23
学习了,很好的
94
好高大上的感觉
96