JAMA Oncol:PET / CT用于局部晚期非小细胞肺癌患者
2017-06-19 zhangfan MedSci原创
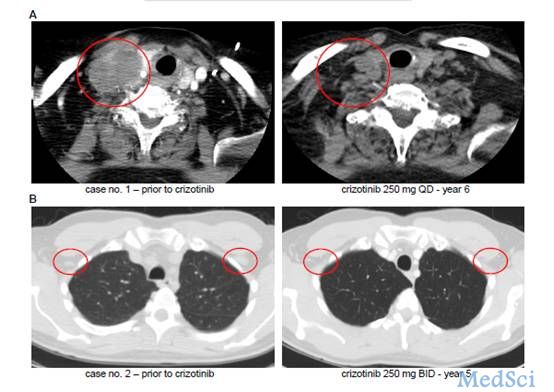
采用升级辐射剂量放疗以及PET检测的方法为无法手术II-III期非小细胞肺癌患者提供了良好的局部肿瘤控制治疗手段
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#局部晚期#
23
#PE#
34
#非小细胞#
27
#Oncol#
32
#肺癌患者#
27
#PET#
32
#局部#
25
#非小细胞肺癌患者#
23
不错的,学习了,谢谢分享!
58
继续学习。
56