Eur Heart J:贫血的房颤患者口服抗凝疗效分析
2019-04-02 xing.T 网络
由此可见,房颤患者贫血较为常见,并伴有大出血和较低的TTR。口服抗凝与更大出血相关,但中度/重度贫血的AF患者卒中/TE风险没有降低。
近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在调查房颤(AF)患者卒中/血栓栓塞(TE)与贫血相关大出血的风险。此外,根据血红蛋白(Hb)水平评估口服抗凝药物(OAC)的疗效和维生素K拮抗剂治疗窗内时间(TTR)。
研究人员通过行政登记数据库,确定了1997年至2012年期间诊断为房颤的所有丹麦患者,并收集了18734名AF患者,这些患者最近的Hb数据可用。研究人员使用多重Cox回归分析来估计风险比并计算卒中/TE和大出血的标准化绝对1年风险。
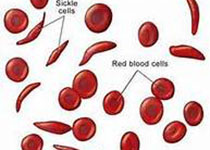
该研究纳入的患者中,3796例(20%)患有轻度贫血(女性Hb为6.83-7.45mmol/L,男性为6.83-8.03mmol/L),2562例(14%)患有中度/重度贫血(Hb<6.83 mmol/L)。与无贫血的受试者相比,中度/重度贫血与大出血风险增加相关,中位TTR降低9.1%。OAC的使用与无贫血患者[标准化绝对1年差异为-2.5%,95%置信区间(CI)为-3.8至-1.7%]或轻度贫血(-2.3%,95%CI为-2.8至-1.8%)卒中/TE风险降低,但不适用于中度/重度贫血患者(0.03%,- 1.8至2.8%,相互作用P=0.01)。口服抗凝药与中度/重度贫血的AF患者中标准化绝对大出血风险增加5.3%(95%CI为2.1-8.7%)相关。
由此可见,房颤患者贫血较为常见,并伴有大出血和较低的TTR。口服抗凝与更大出血相关,但中度/重度贫血的AF患者卒中/TE风险没有降低。
原始出处:
Anders Nissen Bonde.et al.Oral anticoagulation among atrial fibrillation patients with anaemia: an observational cohort study.Eur Heart J.https://doi.org/10.1093/eurheartj/ehz155
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效分析#
33
学习了,谢谢分享
57
学习了,谢谢分享
65
#ART#
24
#HEART#
23
#房颤患者#
25
谢谢梅斯提供这么好的信息,学到很多
36