JACC子刊:热门饮食法再立奇功!可令老年乳腺癌患者心血管疾病风险降低15%!
2022-07-13 MedSci原创 MedSci原创
JACC CardioOncol:限时进食降低老年乳腺癌幸存者的心血管风险:单臂可行性研究
限时进食(TRE)将能量摄入限制在给定的时间窗口内,通常为8小时,然后禁食16小时(16:8 TRE)。这是一种可以改善心脏代谢健康的实用方法,但尚未研究其对癌症人群或心血管疾病(CVD)风险的影响。因此,本项单臂可行性研究,旨在评估8 周 16:8 TRE 对乳腺癌幸存者 (BCS) CVD 风险的初步疗效,以及依从性和安全性。

研究纳入了具有心血管疾病死亡危险因素的BCS:年龄较大(≥60岁),超重或肥胖(体重指数[BMI]≥25 kg / m2),并在1-6年内完成心脏毒性治疗(蒽环类药物)。排除标准包括转移性癌症、使用降脂或降糖药物、磁共振成像 (MRI) 禁忌证、自我报告的糖尿病、过去 3 个月内体重减轻≥15 磅,以及目前正在进行轮班或夜班工作。
参与者在8周内,可在工作日的中午12点到8点之间以及周末的任何时候随意吃东西,这些时间之外只能喝水,黑咖啡或红茶。通过干预前和最后一周进行的24小时饮食记录的3天平均值来评估工作日的卡路里摄入量,并在干预前(基线)和干预后评估初步疗效结局指标。
在228名受邀患者中,22名(10%)入组(平均年龄66±5岁,平均BMI 31±5 kg / m2,n = 1名吸烟者,平均在蒽环类药物治疗后3±1年,没有人接受曲妥珠单抗,50%接受左侧放疗,91%目前服用他莫昔芬和/或芳香酶抑制剂)并完成研究。所有的受试者都完成了研究,对照研究要求,坚持≥16小时的禁食时间的天数占比中位数为98%(范围:85%-100%)。
不良反应轻微(如头痛、易激惹)而短暂(持续5~3小时)。非脂肪体质量没有变化(-0.1±1.6 kg;P=0.76)。卡路里摄入量的中位数为-450千卡(IQR:-765至-28千卡),相对减少22%(P <0.001)。
研究利用了弗雷明汉风险评分来评估未来10年罹患心血管疾病的风险。弗雷明汉CVD风险中位数从10.9%(IQR:8.6%至13.7%)降至8.6%(IQR:7.6%至10.0%),心血管疾病相对风险降低15%,心血管疾病绝对风险降低2%(P = 0.037)。
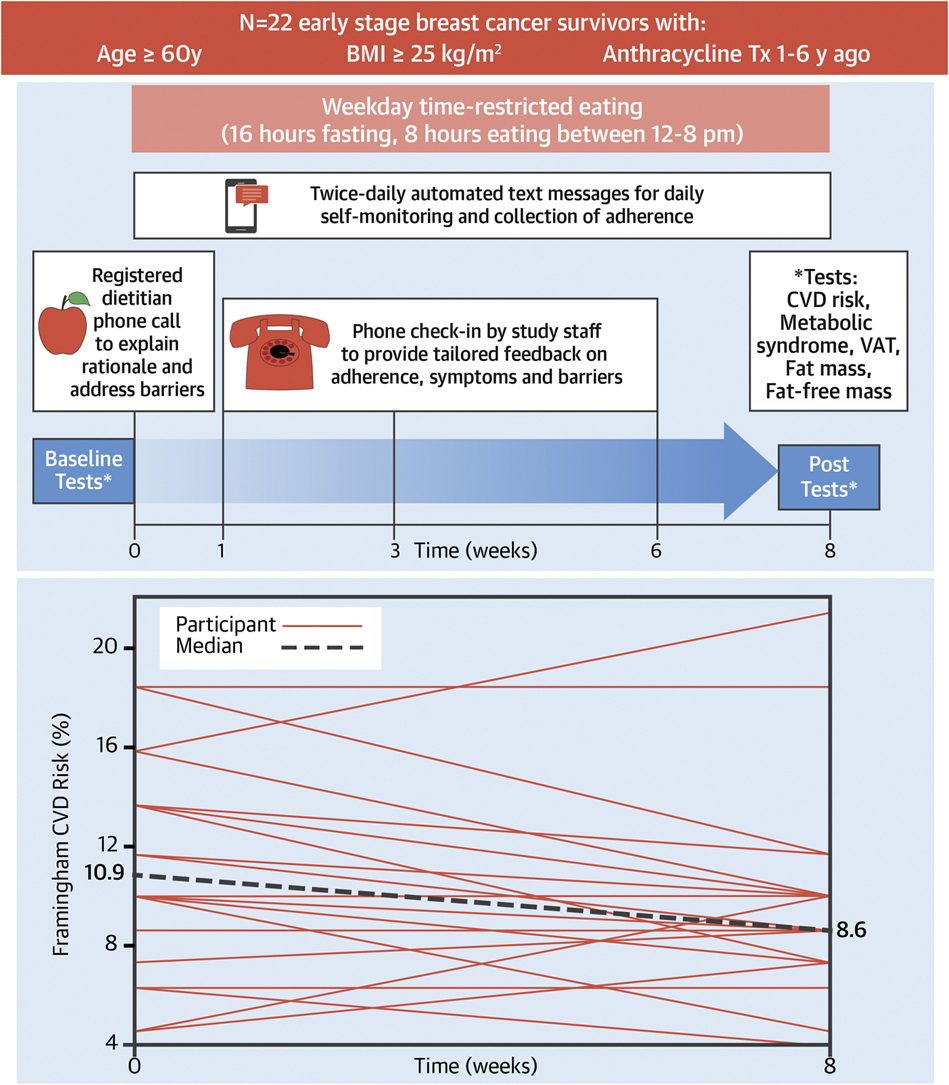
在基线时,22名参与者中有15名(68%)被归类为心脏代谢不健康,根据加拿大心血管学会指南,定义为符合代谢综合征或CVD风险的药物(即他汀类药物)预防性治疗标准。在8周的干预后,15个中有8个(53%)不再符合CVD风险的药物治疗标准或代谢综合征。
研究表明,工作日16:8 TRE是一种非常可行且不良反应轻微的干预措施,可以减少卡路里的摄入量。初步疗效发现包括,对于因超重或肥胖状态、年龄较大和接受蒽环类药物而有心血管疾病死亡风险的乳腺癌幸存者,在短短 8 周内,心血管疾病相对风险降低15%,心血管疾病绝对风险降低2%。
原文来源:
Kirkham AA, Ford KL, Topolnyski J, Da Silva BR, Paterson DI, Prado CM, Joy AA, Boulé NG, Pituskin E, Haykowsky MJ, Thompson RB. Time-Restricted Eating to Reduce Cardiovascular Risk Among Older Breast Cancer Survivors: A Single-Arm Feasibility Study. JACC CardioOncol. 2022 May 17;4(2):276-278. doi: 10.1016/j.jaccao.2022.03.002. PMID: 35818550; PMCID: PMC9270634.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#风险降低#
45
#JACC#
41
#ACC#
48
#疾病风险#
51
#血管疾病#
48
#乳腺癌患者#
42