【病史临床】
患者,男,43岁,体检胸透发现双肺部阴影。无咳嗽咳痰,无胸闷气急,无胸痛不适,无发热盗汗。
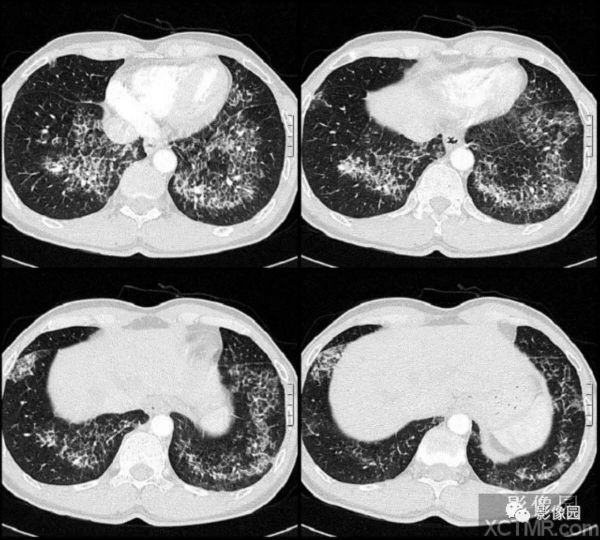
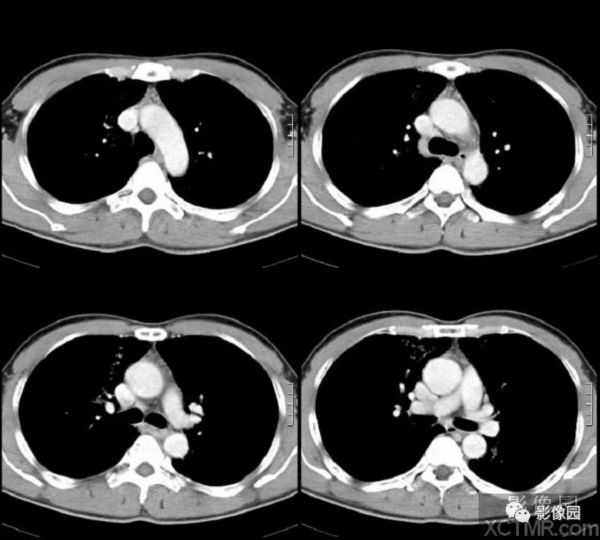
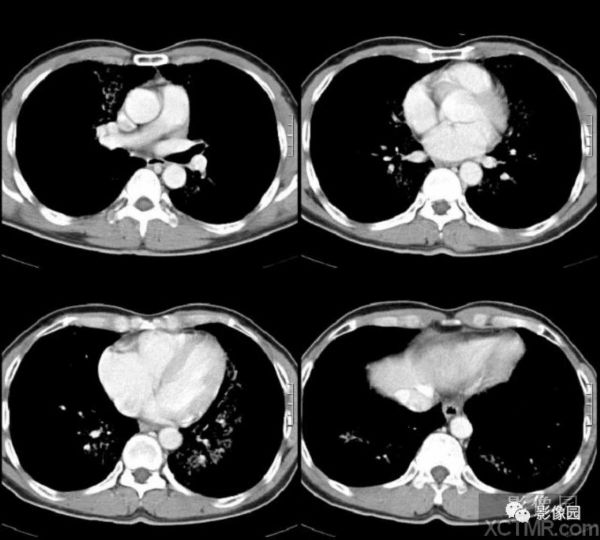
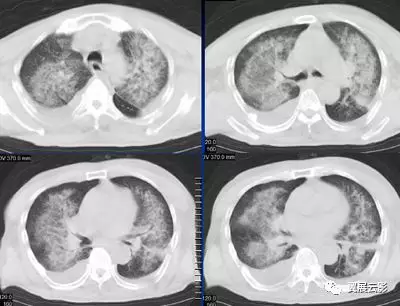
【影像图片】
结果:肺泡蛋白沉着症
点评:肺泡蛋白沉着症(Pulmonary alveolar proteinosis,PAP)是一种原因未明的少见疾病。其特点是肺泡内有不可溶性富磷脂蛋白沉积,临床主要表现为气短、咳嗽和咳痰。男性多于女性,任何年龄均可发病,但30~50岁的中年人常见,约占病例总数的80%。
本病的临床表现差异很大,约1/3病人无任何临床症状,仅在体检时发现,约1/5的病人以继发肺部感染症状为首发表现,约1/2的病人隐袭起病,表现为咳嗽、呼吸困难、乏力,少数病例可有低热和咯血。
双侧对称的磨玻璃影或肺实变,伴有模糊的结节影,以肺门周围或肺下叶为主分布,一些病人可见线状间质影重叠于实变区或磨砂玻璃影上,HRCT上磨玻璃影的边缘常较锐利,似地图样。
多数病例可见细线影形成直径3~10mm的多边形连拱廊样纹路重叠于磨砂玻璃样密度之上,这两种影像的结合表现被描述为“碎石路”,是间隔水肿或正常小叶间隔旁肺泡腔内脂蛋白聚积的结果。
晚期PAP可形成间质纤维化。诊断主要依据胸部影像学检查和支气管肺泡灌洗或纤支镜肺活检。
支气管肺泡灌洗液外观浑浊,呈灰黄色,静置后可分层,则提示有PAP可能,光镜下若见到大量无定型 嗜酸性碎片,PAS染色阳性,则可明确诊断。
经纤支镜肺活检组织若见到典型病理表现也可明确诊断。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CT病例#
33
好好学习天天学习认真学习
59
了解了解.学习学习
65
学习了
61