Hypertension:这种心血管药物影响肥胖高血压患者运动性脂质代谢吗?
2018-01-04 张琪 环球医学
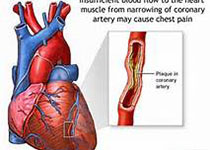
脂肪酸慢性增加会促进心肌脂毒性、血脂异常、胰岛素抵抗和2型糖尿病。相反,降低脂肪酸水平的干预可改善代谢健康。这些观察结果与心血管药物影响脂代谢作用的潜力密切相关。2018年1月,发表在《Hypertension》的一项由德国、荷兰、瑞士和印度科学家进行的多中心、随机、双盲研究,考察了沙库巴曲/缬沙坦对肥胖高血压患者运动性脂质代谢的影响。
沙库巴曲/缬沙坦,一种新型血管紧张素受体脑啡肽抑制剂,近期被批准用于射血分数降低的心衰治疗。脑啡肽降低多种调节脂质代谢的肽,包括利钠肽。在本项研究中,研究人员考察了与代谢中性的氨氯地平相比,沙库巴曲/缬沙坦8周治疗在限定身体运动期间对全身和脂肪组织的脂解作用,以及脂质氧化的影响。
这是一项多中心、随机、双盲、活性对照、平行组研究,纳入了腹部肥胖和中度高血压(平均坐位收缩压≥130~180 mm?Hg)的受试者。使用微量透析和[1,1,2,3,3-2H]-甘油示踪动力学评价静态和运动时的脂解作用。同时,使用间接热量测定同时测量能量消耗和基质氧化情况。并测量血浆非酯化脂肪酸、甘油、胰岛素、血糖、肾上腺素和去甲肾上腺素浓度以及血压和心率。运动提升血浆甘油、游离脂肪酸和间质甘油浓度,并增加甘油呈现率。然而,与氨氯地平相比,运动诱导的脂肪刺激未增强沙库巴曲/缬沙坦的治疗效果。与氨氯地平相比,沙库巴曲/缬沙坦没有改变运动过程中的能量消耗和基质氧化。总之,为期8周的沙库巴曲/缬沙坦治疗没有使肥胖高血压患者的运动诱导脂解或基质氧化发生相关变化,表明其有益的心血管效应不能通过运动过程中脂代谢的变化来解释。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PE#
38
#心血管药物#
39
#TENS#
37
#运动性脂质代谢#
30
#脂质代谢#
50
#高血压患者#
33
#Hypertension#
24
学习一下
39