Nature:前列腺癌研究、诊断和治疗的现状和发展前景
2015-12-25 MedSci MedSci原创
只要寿命足够长,大多数男性都会发展出前列腺癌。在全球范围内前列腺癌是男性第二常见的癌症,在某些地区它甚至坐上了第一把交椅。最近Nature杂志发布了前列腺癌专题,通过一系列文章全面介绍了前列腺癌研究、诊断和治疗的现状和发展前景,探讨了该领域的一些争议问题。 前列腺癌分子病因 前列腺癌基因组复杂性,也成为2015年研究焦点(The genomic complexity of pr
只要寿命足够长,大多数男性都会发展出前列腺癌。在全球范围内前列腺癌是男性第二常见的癌症,在某些地区它甚至坐上了第一把交椅。最近Nature杂志发布了前列腺癌专题,通过一系列文章全面介绍了前列腺癌研究、诊断和治疗的现状和发展前景,探讨了该领域的一些争议问题。
前列腺癌与炎症
当男性的生育黄金期过去之后,前列腺会出现一些不太正常的行为,这种情况的第一个迹象往往是炎症。正因如此,前列腺炎有时(并不总是)是癌症的先兆。炎症与癌症之间的相互作用,一直是科学家们关注的热点(Microbiology: Inflammatory evidence)。
筛查争议
近年来,前列腺癌筛查引起了很大的争议。前列腺特异性抗原PSA是一种前列腺生产的蛋白,如果存在前列腺肿瘤,血液中的PSA水平就会比较高。PSA血检可以在更早、更好治疗的阶段发现癌症,为前列腺癌治疗做出了很大的贡献。然而,人们慢慢发现PSA血检会给出误导性的结果。这种方法检出的不少肿瘤就算不治疗也是安全的。(Screening: Diagnostic dilemma)
为此研究人员正在寻求PSA以外的其他生物指标,以便获得更可靠的检测结果,鉴别那些真正危险的前列腺癌和真正需要治疗的癌症患者。“Prognosis: Proportionate response”这篇文章详细介绍了这方面的进展。
治疗策略
在很多情况下,前列腺癌最好的选择是保持警惕。对于比较不具侵袭性的前列腺癌来说,“积极监控”正在成为新的口号。越来越多的医生开始青睐这种更为保守的治疗方法,密切监控肿瘤发展,只在疾病恶化的时候进行治疗。这能使前列腺患者在真正需要的时候享受最新的医疗成果。(Treatment: When less is more)
如果前列腺手术已经无可避免,手术机器人正在使患者更加安全。澳大利亚墨尔本Peter MacCallum癌症中心的机器人手术主管Declan Murphy,在一篇访谈文章中畅谈了这一技术的应用和现状。(Q&A: Declan Murphy)
新的探索
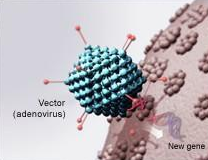
可惜的是,前列腺癌疫苗依然希望渺茫。唯一通过批准的前列腺癌免疫疗法(sipuleucel-T),只能帮助患者延长几个月生命,而且价格非常昂贵。研究人员正在重点开发联合疗法,希望通过互补途径刺激免疫系统,帮助更多前列腺患者延长生命。举例来说,可以把检验点疗法与靶标肿瘤缺氧的药物一起使用。(Therapy: An immune one–two punch)
第二个问题:PSA筛查足够有效吗?
第三个问题:移去前列腺癌或放疗是安全的吗?
第四个问题:晚期前列腺癌如何处理?如何延长生存期?
(Prostate cancer: 4 big questions)本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发展前景#
23
#Nat#
32
是一篇不错的文章
165
这篇文章有一定深度
121
目前对于晚期前列腺癌还没有确切有效廉价的治疗方法,期待将来精准治疗应用于临床。
101
牛
166
(⊙_⊙)
136
看了后,原文更好理解
61
还是得看原文
64
有争议就有进步
130