Cell Stem Cell:外膜间充质干细胞样细胞在血管钙化中的作用研究
2017-03-19 MedSci MedSci原创
来自哈佛大学医学院的医师科学家Rafael Kramann对基础及转化医学研究都有广泛的兴趣,他的研究方向是原位或循环间充质干细胞在心脏和肾脏纤维化,血管内环境稳态和疾病中的作用。近日发表题为<外膜间充质干细胞样细胞是血管平滑肌细胞的祖细胞并驱动慢性肾脏病血管钙化>于cell stem cell,该杂志目前影响因子为22.387。
来自哈佛大学医学院的医师科学家Rafael Kramann对基础及转化医学研究都有广泛的兴趣,他的研究方向是原位或循环间充质干细胞在心脏和肾脏纤维化,血管内环境稳态和疾病中的作用。近日发表题为<外膜间充质干细胞样细胞是血管平滑肌细胞的祖细胞并驱动慢性肾脏病血管钙化>于cell stem cell,该杂志目前影响因子为22.387。
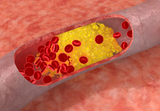
间充质干细胞样细胞主要驻留在血管壁,但对于它们在血管再生、血管疾病中的作用了解甚少。本研究作者发现位于动脉外膜的Gli1 +细胞是血管平滑肌细胞的祖细胞,并促进新生内膜形成和股动脉急性损伤后的血管修复。谱系追踪显示在ApoE敲除小鼠慢性肾脏疾病动脉粥样硬化和动脉硬化期间外膜Gli1 + 间充质干细胞样细胞迁移到中膜和新生内膜。数据表明Gli1 +细胞是中膜和内膜钙化期间成骨细胞样细胞的主要来源。在诱导肾损伤之前先敲除Gli1 +细胞显着降低血管钙化的严重程度。
这些发现提示Gli1 +细胞是急性和慢性损伤时血管重塑的关键外膜祖细胞,表明它们可能是缓解血管钙化的关键靶标。
原始出处:Kramann R, Goettsch C,et al. Adventitial MSC-like Cells Are Progenitors of Vascular Smooth Muscle Cells and Drive Vascular Calcification in Chronic Kidney Disease. Cell Stem Cell. 2016 Nov 3;19(5):628-642.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#stem cell#
34
#CEL#
25
#间充质干细#
27
#Cell#
26
#STEM#
32
签到学习了很多。
76