European Radiology:他来了!可预测基底动脉闭塞性卒中患者预后的新的影像学评分
2022-08-02 shaosai MedSci原创
最近,有学者提出了一个由ASPECTS和准分子组成的联合影像学评分对基线前循环卒中患者进行广泛筛查,并观察到该评分(即ASCO评分)表现出比CT灌注派生的参数更优的诊断能力。
总所周知,基底动脉闭塞(BAO)患者的临床症状种类繁多,对其进行准确的神经系统评估十分具有挑战性。因此,使用神经影像学进行诊断及评估不仅可以对患者进行适当的治疗,还可以早期发现如恶性小脑水肿(MCE)等严重并发症的发生。与前循环缺血性卒中相比,BAO影像学评分的使用在日常临床实践中尚未确立。
然而,后循环急性卒中预后早期CT评分(pcASPECTS)提出的BAO卒中患者入院时CT低钙化程度或侧支循环状态评分是否可以作为预测结果和并发症的工具目前尚未评估,但最近的研究表明,pcASPECTS较高的患者更适合选择血栓切除术进行治疗。
最近,有学者提出了一个由ASPECTS和准分子组成的联合影像学评分对基线前循环卒中患者进行广泛筛查,并观察到该评分(即ASCO评分)表现出比CT灌注派生的参数更优的诊断能力。但据我们所知,尚未有研究为BAO卒中患者的评估类似设计的评分。
近日,发表在European Radiology杂志的一项研究利用pcASPECTS和后循环栓塞(pcASCO)的综合评分评估了BAO患者第90天的功能预后和48小时MCE发生率之间的关系,为临床准确评估BAO患者的病情及治疗预后提供了参考依据。

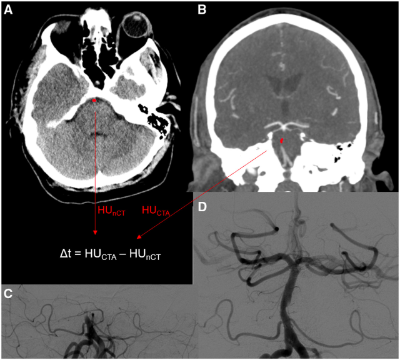
本研究对在两个综合卒中中心接受多模态CT检查并在入院时接受血栓切除术的急性BAO患者进行了分析。在pcASPECTS中加入van der Hoeven等人的后循环旁路评分,并将pcASCO定义为一个20分的评分。进行多变量逻辑回归分析以预测第90天的功能预后独立性,使用改良的Rankin量表评分进行评估,并以既定的Jauss量表评分作为终点预测后续CT中MCE的发生情况。
本研究共纳入118名患者,其中84人(71%)成功进行了血栓切除术。根据ROC曲线分析,pcASCO≥14的功能独立分类比pcASPECTS(AUC:0.83,95%CI:0.71-0.91)具有更高的鉴别力(AUC:0.74)。在多变量逻辑回归分析中,pcASCO与功能独立(aOR:1.91,95%CI:1.25-2.92,p = 0.003)和MCE(aOR:0.71,95%CI:0.53-0.95,p = 0.02)明显独立相关。
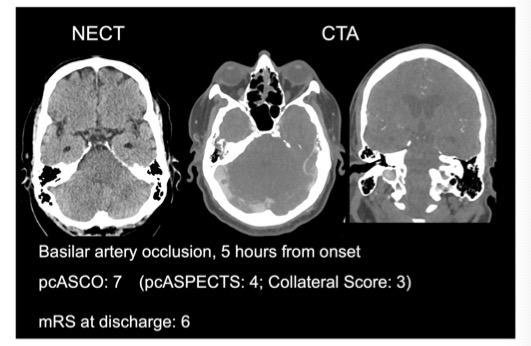
图 一个pcASCO评分很低、预后很差的患者示例,该急性基底动脉闭塞的患者在症状出现5小时后被评估为pcASCO评分为7分(pcASPECTS 4分+后循环侧支3分)
本研究证明了pcASCO评分对BAO患者预后分类的极高诊断能力,本表明该评分系统可作为MCE的一项有价值的预测指标。本研究同时表明,该评分可在不确定的情况下对BAO卒中患者进行血栓切除术的筛选,并可对患者预后进行预测。
原文出处:
Gabriel Broocks,Lukas Meyer,Tobias D Faizy,et al.New imaging score for outcome prediction in basilar artery occlusion stroke.DOI:10.1007/s00330-022-08684-9
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#基底动脉闭塞性卒中#
38
#闭塞性卒中#
50
#卒中患者#
39
#患者预后#
37
#PE#
32
#动脉闭塞#
45
#基底动脉#
36