一项基于中国慢性病前瞻性研究项目的新分析提示,静息心率越快,肺心病发生风险越高,当静息心率>75次/分时,心衰风险也显著增加。该研究于2004~2008年从中国10个地理位置不同的地区纳入近50万名成年人,其平均年龄为51.7岁,60%为女士。
这些人基线均无心脏病病史,也没有服用β受体阻滞剂;基线平均静息心率为79次/分,其中男士和女士分别为78次/分、80次/分,随着年龄增长心率下降,大约每10年下降1次/分。
中位随访11年期间,6082人出现心衰,5572人出现肺心病。仅4.7%的肺心病是在诊断心衰后发生的;心衰患者中,也仅有5.2%先诊断肺心病。
分析显示,平素静息心率与心衰之间呈J型曲线关系,与肺心病之间呈对数线性关系。平素静息心率每增加10次/分,肺心病发生风险增加74%。但只有当静息心率>75次/分时,每增加10次/分,心衰风险增加25%。进一步校正糖尿病和高血压后,静息心率>75次/分时,每增加10次/分,心衰风险大约减半。

这一研究结果与既往发表的弗明汉心脏研究相似。后者显示,静息心率>80次/分时,每增加10次/分,心衰风险增加14%。
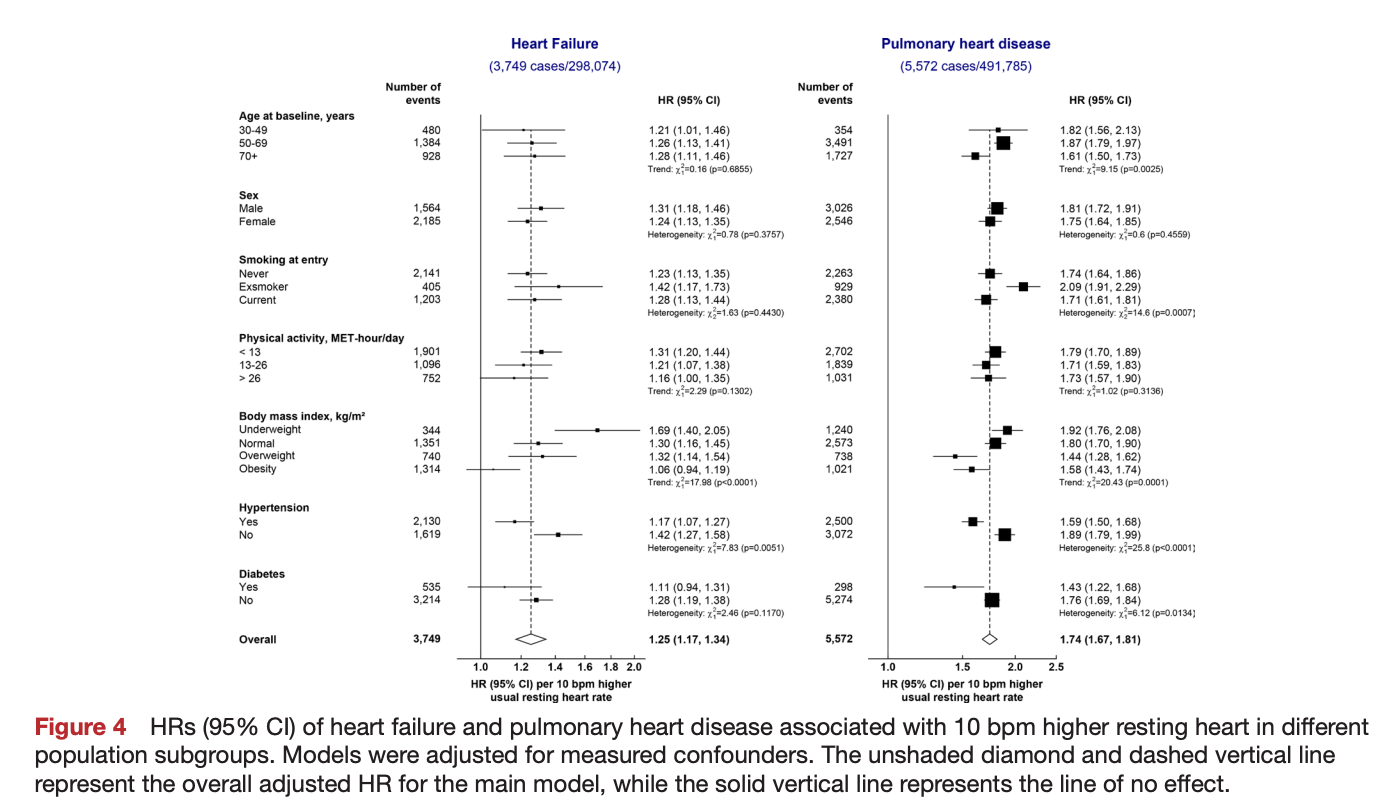
作者指出,该研究结果提示,静息心率与右心衰的关系可能比与左心衰的关系更强。
对于慢阻肺患者,很多临床医生不愿意用β受体阻滞剂,该研究表明,从人群层面来看,降低静息心率可能会显著降低心衰和肺心病的发病和死亡风险,但需要进一步验证。该研究结果支持进一步开展研究来评估β受体阻滞剂对肺心病的疗效,以及探索慢阻肺患者心脏并发症的预防策略。
来源:Resting heart rate and risk of left and right heart failure in 0.5 million Chinese adults. Open Heart, 2022, 9(1): e001963.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#前瞻性#
38
#前瞻性研究#
38
#PE#
29
学习
40
#慢性病#
75
#ART#
33
#HEART#
31