Clin Gastroenterol Hepatol:溃疡出血后停阿司匹林增心血管死亡风险
2013-01-06 Clin Gastroenterol Hepatol CMT
《临床胃肠病学和肝病学》杂志1月刊发的一项研究结果显示,在因消化性溃疡出血住院且正在接受低剂量阿司匹林治疗的患者中,出院后停用阿司匹林的患者在出院后不久发生死亡或心血管(CV)事件的风险,是出院后重新使用阿司匹林的患者的6倍(Clin. Gastroenterol. Hepatol. 2013;11:38-42)。 这项研究由斯德哥尔摩卡罗林斯卡研究所的Maryam Derogar女士及
《临床胃肠病学和肝病学》杂志1月刊发的一项研究结果显示,在因消化性溃疡出血住院且正在接受低剂量阿司匹林治疗的患者中,出院后停用阿司匹林的患者在出院后不久发生死亡或心血管(CV)事件的风险,是出院后重新使用阿司匹林的患者的6倍(Clin. Gastroenterol. Hepatol. 2013;11:38-42)。
这项研究由斯德哥尔摩卡罗林斯卡研究所的Maryam Derogar女士及其同事进行,研究对象为2007~2010年间接受治疗的118例上消化道出血成人患者。所有患者存在内镜证实的消化性溃疡,并且在住院时正在接受低剂量阿司匹林治疗(75 mg或160 mg/d)。该研究排除了那些除了消化性溃疡出血之外还存在其他出血源(如食管静脉曲张或血管发育不良)的患者。
40%(47例)患者永久停用阿司匹林。40%(48例)在出院后立即再次开始使用阿司匹林,其余20%(23例)患者在出院后2天至2个月(中位值为1周)再次接受阿司匹林治疗。
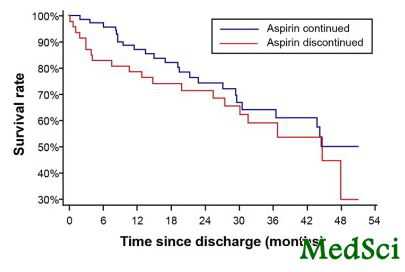
在中位随访2年期间,37%(44例)患者发生死亡或急性心血管事件。停用阿司匹林患者在随访最初6个月内的死亡或急性CV事件发生率是再次使用阿司匹林患者的6倍,危险比(HR)为6.8。研究者对酒精滥用、慢性缺血性心脏病(心绞痛)、慢性心力衰竭、既往心肌梗死、房颤、既往卒中或TIA、慢性肾功能衰竭、糖尿病、COPD和癌症等潜在混杂因素进行了校正。进一步分析显示,仅原有CV合并症的患者在随访最初6个月内的死亡和急性CV事件发生率增加,而在无CV合并症的患者中未观察到增加的现象。在26例停用阿司匹林的此类患者中,该发生率为31%,而在50例再次使用阿司匹林的患者中,发生率仅为8%。
随访6个月后,停用阿司匹林的患者与再次使用阿司匹林的患者的死亡和急性CV事件发生率无显著差异。6%的患者在随访期间因复发性消化性溃疡出血而再次住院。无患者因再次出血而死亡。
这些结果证实了既往一项随机临床研究的结果,后者显示,永久停用阿司匹林的患者在随访2个月内的死亡率是继续使用阿司匹林的患者的8倍(Ann. Intern. Med. 2010;152:1-9)。
研究者表示,本文研究中的所有死亡或急性CV事件均发生在年龄≥64岁的患者中,因此研究结果可能不完全适用于年龄较小的患者,同时提示老年患者可能更倾向于停止阿司匹林治疗。对于发生消化性溃疡出血且存在CV风险的老年患者,不应永久停用阿司匹林,而应在治疗出血后继续使用阿司匹林。鉴于阿司匹林的致溃疡性,强烈建议联用质子泵抑制剂这样的抑酸剂。
Derogar女士声明无经济利益冲突。一位研究者声明从Olle Engkvist Byggmastare基金会获得奖学金。
专家视点:溃疡出血后停用阿司匹林,风险大于获益
威斯康辛大学医学与公共卫生学院的临床内科学教授NIMISH VAKIL表示,在冠状动脉疾病或脑血管疾病患者发生消化道出血并进行内镜治疗时,许多消化科医生面临的问题就是是否应再次使用阿司匹林和(或)氯吡格雷,如果再次使用,应何时使用。这些患者常由于高龄和合并症而具有较高的出血相关并发症风险,并且由于晚期血管疾病,发生心血管或脑血管并发症的风险也较高。临床医生有4种方案可选:永久停用阿司匹林和氯吡格雷;停用阿司匹林,再次使用氯吡格雷;在达到内镜下止血后再次使用这两种抗血小板药物;或在达到内镜下止血后暂停使用抗血小板药7~10天。
尽管目前尚无完整且有效的证据基础来指导当前临床实践,但根据近期研究可归纳出重要的几点。上述研究显示,完全停用阿司匹林与死亡或CV并发症高发生率相关,而另一方面,在继续使用阿司匹林的患者中再出血较罕见。近期一项纳入接受低剂量阿司匹林治疗的消化道出血患者的随机对照研究显示,内镜下止血后继续使用阿司匹林的患者组的30天内复发性溃疡出血发生率为10.3%,而内镜下止血后停用阿司匹林的安慰剂组的该发生率为5.4%。阿司匹林组的全因死亡率低于安慰剂组(1.3% vs. 12.9%)(Ann. Intern. Med. 2010;152:1-9)。其他研究显示,再次使用阿司匹林及合用质子泵抑制剂的效果优于单用氯吡格雷。
至于内镜下止血后是应该立即再次使用还是暂停使用阿司匹林或氯吡格雷一段时间,目前尚缺乏指导依据。具体的治疗决定可能应取决于出血的程度、基础CV和脑血管疾病及合并症的严重程度。现有证据表明,在使用阿司匹林治疗CV或脑血管疾病的患者中,停用阿司匹林是不明智的,会增加不良结局的发生率。

Background & Aims
Little is known about how discontinuation of low-dose aspirin therapy after peptic ulcer bleeding affects patient mortality or acute cardiovascular events.
Methods
We performed a retrospective cohort study by using data from patients who received low-dose aspirin therapy and were treated for bleeding peptic ulcers between 2007 and 2010 at Karolinska University Hospital, Stockholm, Sweden. We used a multivariable Cox regression model to adjust for potential confounders and analyze associations between discontinuation of low-dose aspirin therapy at discharge, death, and acute cardiovascular events.
Results
Of the 118 patients who received low-dose aspirin therapy, the therapy was discontinued for 47 (40%). During a median follow-up period of 2 years after hospital discharge, 44 of the 118 patients (37%) either died or developed acute cardiovascular events. Adjusting for confounders, patients with cardiovascular comorbidities who discontinued low-dose aspirin therapy had an almost 7-fold increase in risk for death or acute cardiovascular events (hazard ratio, 6.9; 95% confidence interval, 1.4–34.8) compared with patients who continued this therapy during the first 6 months of the follow-up period. A corresponding association was not observed among patients without cardiovascular comorbidities when the study began.
Conclusions
In patients with cardiovascular disease, discontinuation of low-dose aspirin therapy after peptic ulcer bleeding increases risk of death and acute cardiovascular events almost 7-fold.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Gastroenterol#
22
#AST#
31
#GAS#
33
#死亡风险#
23
#EPA#
23
#心血管死亡#
18
#心血管死亡风险#
28