STM:新型水凝胶可能改变心肌愈合方式,还你一颗健康的心脏
2021-02-20 MedSci原创 MedSci原创
由于心肌不可逆转的损伤,缺血性心脏病是导致死亡的主要原因。过去十年,非透壁性心肌梗死的发病率在临床上有所增加,目前尚无可防止梗塞区域进一步功能恶化的治疗方法。
由于心肌不可逆转的损伤,缺血性心脏病是导致死亡的主要原因。过去十年,非透壁性心肌梗死的发病率在临床上有所增加,目前尚无可防止梗塞区域进一步功能恶化的治疗方法。

Pixabay
近日,发表在 Science Translational Medicine 杂志的研究报告了一种可注射的水凝胶,可以帮助修复和防止心脏病发作后心肌的进一步损伤。
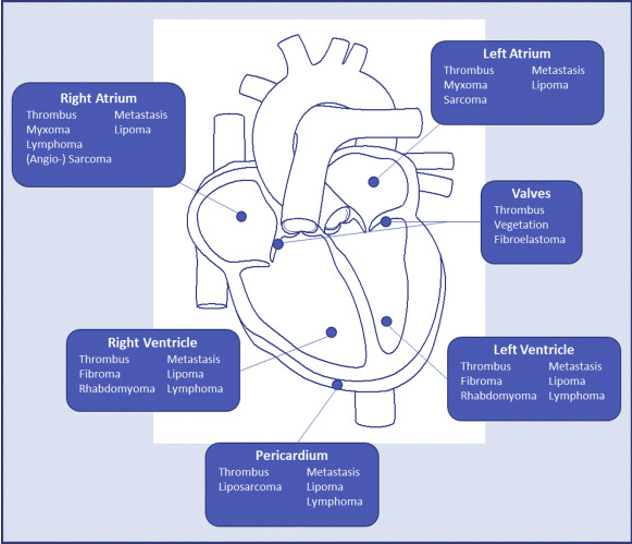
这种可注射的水凝胶是基于一种独特的生物材料---弹性蛋白(ELN)重组蛋白,可以更好的模拟心肌梗死后心脏周围的环境。这种水凝胶包括细胞粘附和蛋白酶裂解位点的功能域,对心肌梗死后过度表达的基质金属蛋白酶具有高度敏感性。
研究人员发现,心肌内注射可降解的ELRs-水凝胶使干预后21天的射血分数功能完全恢复。与未经治疗的动物相比,ELRs-水凝胶处理的缺血性核心区域观察到了更少的纤维化和更多的血管生成。GATA4+导致纤维化基因的表达降低,减少心脏病发作纤维化,并改善心脏病发作模型的心脏功能。
研究人员还观察到,注射凝胶后,心肌细胞的保存率和存活率上升。因此,通过及时注射ELRs-水凝胶在临床相关的透壁性心肌梗死模型中获得的效益,然后进一步的临床转化。
综上,通过调节缺血核心和明显的功能恢复来保存边界区的心肌细胞,及时注射水凝胶所获得心脏功能性益处。目前,研究人员正在不同的临床环境中注射ELRs-水凝胶应用于,并将随后转化为临床试验。
原始出处
Paolo Contessotto et al. Elastin-like recombinamers-based hydrogel modulates post-ischemic remodeling in a non-transmural myocardial infarction in sheep, Science Translational Medicine (2021). DOI: 10.1126/scitranslmed.aaz5380
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#STM#
51
#水凝胶#
65
#凝胶#
41
学习了
102