Gastroenterology:无菌粪便滤液同样能治疗艰难梭菌感染吗?
2016-11-20 MedSci MedSci原创
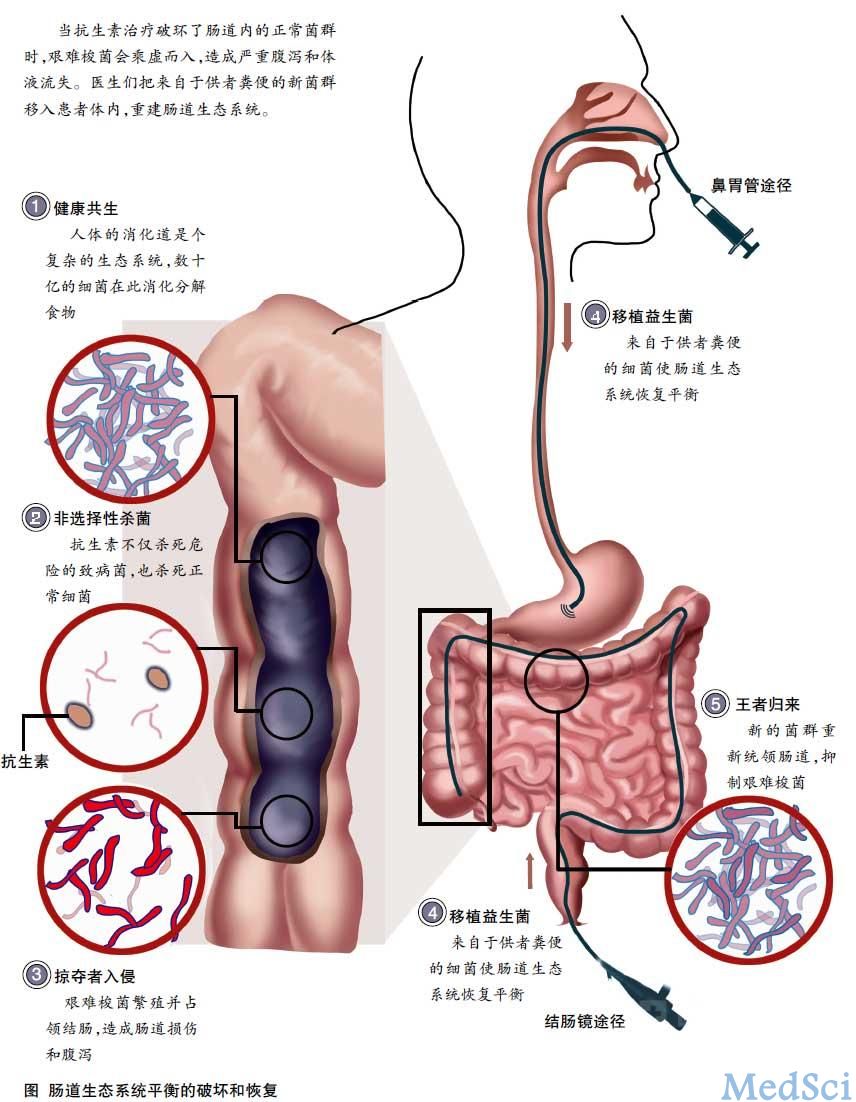
粪便菌群移植(FMT)是复发性艰难梭菌感染(CDI)的一个非常有效的治疗方案。研究目的是,调查无菌粪便滤液(含细菌碎片、蛋白质、抗菌化合物、代谢产物和寡核苷酸/ DNA)而不是完整的微生物,对CDI的治疗是否有效。 我们进行了一项病例系列研究,观察粪便滤液转移(FFT)对5例症状性慢性复发性CDI患者的疗效。患者随访6个月到33个月。FFT前、后1周和6周采集患者的粪便标本,比较捐赠者和患者
粪便菌群移植(FMT)是复发性艰难梭菌感染(CDI)的一个非常有效的治疗方案。研究目的是,调查无菌粪便滤液(含细菌碎片、蛋白质、抗菌化合物、代谢产物和寡核苷酸/ DNA)而不是完整的微生物,对CDI的治疗是否有效。
我们进行了一项病例系列研究,观察粪便滤液转移(FFT)对5例症状性慢性复发性CDI患者的疗效。患者随访6个月到33个月。FFT前、后1周和6周采集患者的粪便标本,比较捐赠者和患者的微生物、病毒和蛋白质等。
所有5例患者的大便习惯均恢复正常,CDI症状的消除最短时间为6个月。选择性FFT滤液的蛋白质组分析没有发现与疗效相关的明显候选蛋白质。16S rRNA基因测序显示了细菌DNA的多样性。滤液病毒样颗粒分析发现,CDI症状的减少与复杂的噬菌体有关。受者粪便样品的细菌和病毒的系统发育分析显示了FFT后微生物和病毒群落结构的纵向变化。
5例CDI患者的初步调查显示,供体粪便提取的无菌滤液,而不是粪便菌群,足以恢复患者的正常大便习惯和消除症状。这一发现表明,细菌成分、代谢产物或噬菌体介导FMT的许多疗效。
原始出处:
Stephan J. Ott,et al.Efficacy of Sterile Fecal Filtrate Transfer for Treating Patients With Clostridium difficile Infection.Gastroenterology.Articles in Press
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#GAS#
33
#AST#
27
#Gastroenterol#
30
#粪便#
33
#Gastroenterology#
29