N Engl J Med:本妥昔单抗联合化疗晚期霍金淋巴瘤一线治疗重大突破
2018-02-02 慧语 肿瘤资讯
2018开年,《NEJM》正式发表了晚期霍金淋巴瘤一线治疗的一项突破性研究,研究人员报道了Ⅲ期ECHELON-1临床试验的数据。该项试验评估了Brentuximab+Vedotin作为一线联合化疗方案用于未治疗的晚期霍奇金淋巴瘤(HL)患者的疗效和安全性。
2018开年,《NEJM》正式发表了晚期霍金淋巴瘤一线治疗的一项突破性研究,研究人员报道了Ⅲ期ECHELON-1临床试验的数据。该项试验评估了Brentuximab+Vedotin作为一线联合化疗方案用于未治疗的晚期霍奇金淋巴瘤(HL)患者的疗效和安全性。
背 景
本妥昔单抗(Brentuximab Vedotin),商品名Adcetris,是一种抗体药物耦合物(ADC),能够特异结合表达CD30抗原的肿瘤细胞,而CD30抗原是霍奇金淋巴瘤(HL)和间变性大细胞淋巴瘤(ALCL)的明确生物标志物,在肿瘤生长和存活方面发挥重要作用。美国FDA于2011 年 8 月 19 日批准其上市,用于治疗复发和难治性霍奇金淋巴瘤。
方 法
这是一项开放性,多中心,随机的3期临床试验,接受研究对象为未经治疗的III期或IV期经典霍奇金淋巴瘤患者,2012年11月19日至2016年1月13日期间,共有来自21个国家218个中心的1334名患者按1:1比例随机分配到试验组和对照组。其中试验组664例患者接受本妥昔单抗,多柔比星,长春碱和达卡巴嗪(A + AVD)治疗方案;对照组670例患者接受多柔比星,博来霉素,长春碱和达卡巴嗪(ABVD)治疗方案。主要研究终点为由独立评审委员会决定的无进展生存期PFS(终点事件包括:进展、死亡、不完全缓解或接受其他抗癌治疗)。次要研究终点为总体生存OS。
结 果
① 疗效:PFS、OS
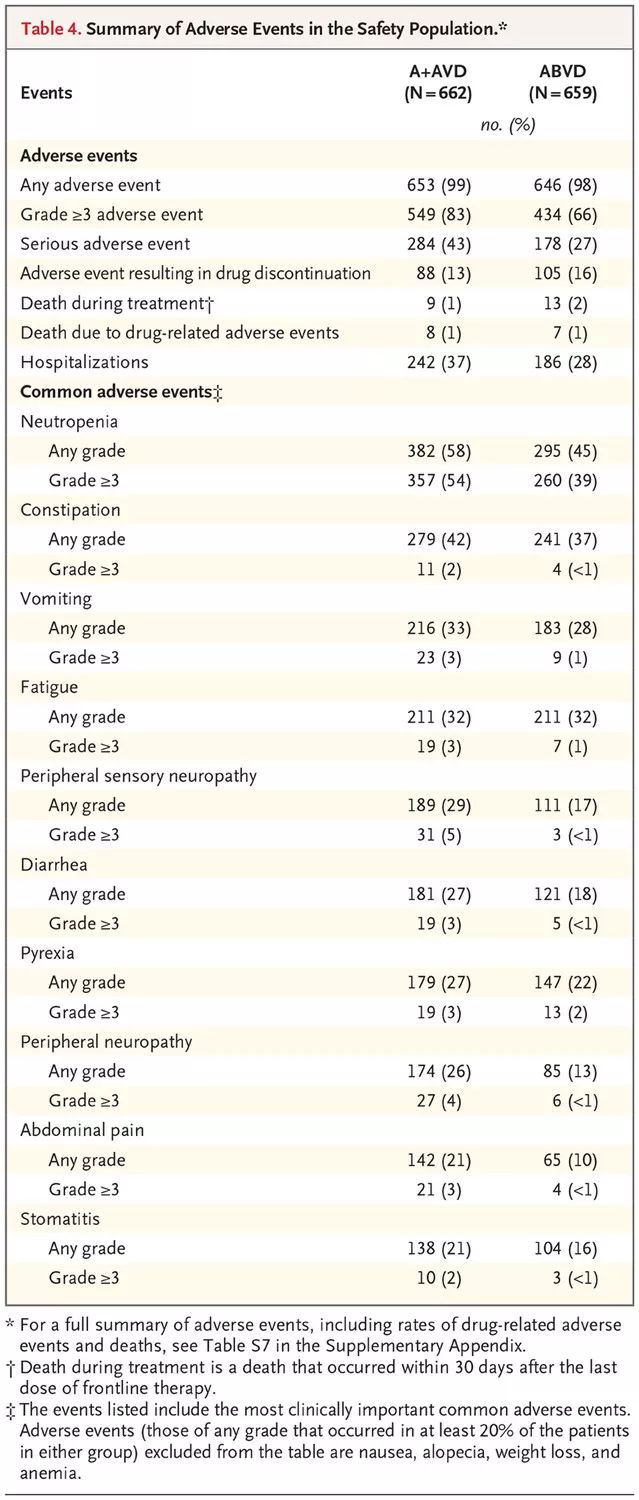
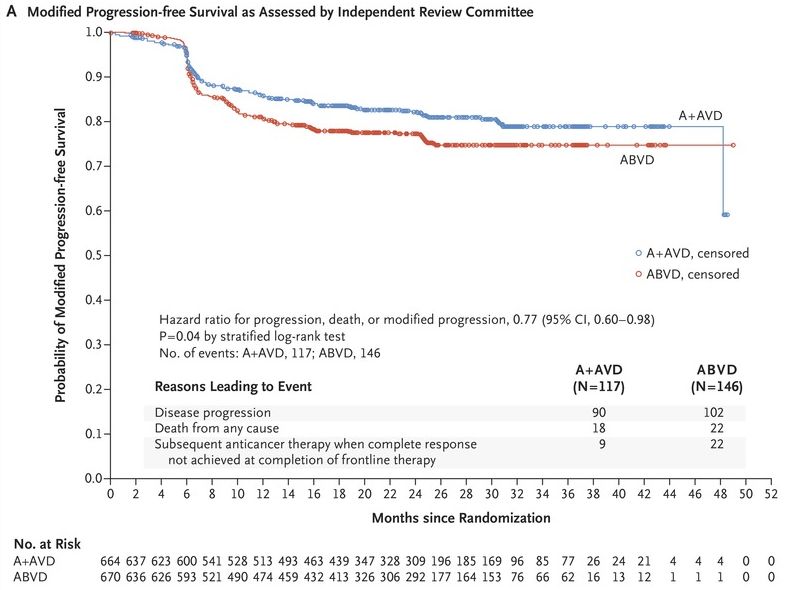
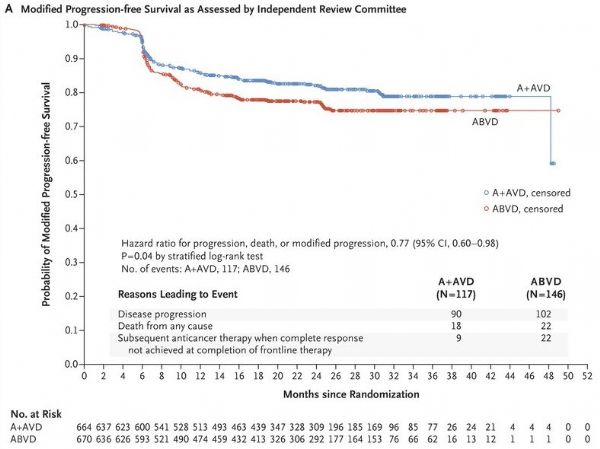
入组患者的中位随访时间为24.6个月。A + AVD和ABVD组的2年PFS分别为82.1%(95%可信区间CI:78.8~85.0)和77.2%(95% CI ,73.7~80.4),相差4.9%(HR=0.77; 95% CI,0.60~0.98; P = 0.03)(图1)。其中A + AVD组有28例死亡,ABVD组有39例死亡,OS的HR=0.72 (95% CI :0.44~1.17; P = 0.19)。
图1 A+AVD和ABVD两组的PFS生存曲线
② 亚组分析
几乎在所有的亚组中都一致显示A + AVD组PFS获益(HR<1)的趋势(图2)。
图2 亚组分析森林图
③ 安全性
接受A + AVD的患者中有58%发生了中性粒细胞减少,ABVD组中性粒细胞减少的比例在45%。出现周围神经病变的比例在 A + AVD组和ABVD组中分别为67%和43%; 但A + AVD组中67%的周围神经病变患者在最后一次随访中有改善或好转。 3级及以上的肺毒性报告在接受A + AVD的患者中不到1%,ABVD组中有3%。治疗期间发生的死亡,A + AVD组中9例有7例是与中性粒细胞减少症相关,而ABVD组中13例有11例与肺毒性相关(表1)。
表1 两组患者不良事件描述
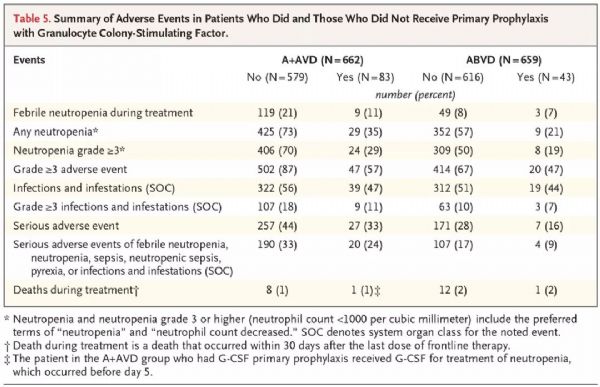
④ 接受G-CSF预防治疗的安全性
在入组达到76%时,经独立数据监察委员会讨论,建议对后面随机到A+AVD组的患者将给予粒细胞集落刺激因子(G-CSF)作为一级预防,在治疗开始的第5天使用G-CSF,因为该组发热性嗜中性白血球减少症的发生率较高。 在A + AVD组中,83例接受G-CSF预防治疗的患者发生发热性嗜中性白血球减少症的比例为11%,比未接受预防治疗的患者低了10个百分点(11% [9/83] VS. 21% [119/579])(表2)。
表2 两组中接受与不接受G-CSF预防治疗的患者不良事件的描述
结 论
A + AVD治疗晚期霍奇金淋巴瘤患者的疗效优于ABVD。治疗两年后,进展、死亡或不完全缓解的联合风险降低4.9%。ECHELON-1研究是近30年来HL领域的一次重大突破。A+AVD方案提高了患者持久缓解的比例,同时毒性未显着增加。这一新方案为晚期HL患者一线治疗的推广提供有力佐证。
原始出处:Joseph M. Connors, M.D., Wojciech Jurczak, M.D., Ph.D., David J. Straus, M.D., et al. Brentuximab Vedotin with Chemotherapy for Stage III or IV Hodgkin’s Lymphoma. N Engl J Med 2018; 378:331-344
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Eng#
31
#Engl#
34
#联合化疗#
34
#Med#
0
#本妥昔单抗#
24
#霍金#
32