Neural Regen Res.:脉络膜上腔注射酮咯酸氨丁三醇后神经节细胞的变化
2013-01-09 EurekAlert!中文 EurekAlert!中文
酮咯酸氨丁三醇对眼底疾病如脉络膜新生血管,视网膜新生血管,糖尿病视网膜眼底病变及黄斑囊样水肿的治疗有较大潜力,但在给药方式和剂量的应用上有很多争议。《中国神经再生研究(英文版)》杂志于2012年12月35期出版的一项关于“Suprachoroidal injection of ketorolac tromethamine does not cause retinal damage”的研究显示,给正
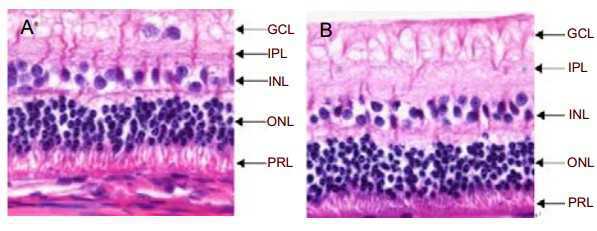
酮咯酸氨丁三醇对眼底疾病如脉络膜新生血管,视网膜新生血管,糖尿病视网膜眼底病变及黄斑囊样水肿的治疗有较大潜力,但在给药方式和剂量的应用上有很多争议。《中国神经再生研究(英文版)》杂志于2012年12月35期出版的一项关于“Suprachoroidal injection of ketorolac tromethamine does not cause retinal damage”的研究显示,给正常新西兰大白兔右眼脉络膜上腔注射3000,6000μg的酮咯酸氨丁三醇后,其视网膜电图波形、振幅和潜伏期均未出现异常改变,兔视网膜神经节细胞层、内网状层、内核层、外核层和光感受器层细胞形态和排列未出现明显变化,视网膜形态结构也未出现明显变化。这项研究结果说明,剂量为3000,6000μg的酮咯酸氨丁三醇在兔眼脉络膜上腔单次注射是安全的,且给药方式也是安全的。

doi:10.3969/j.issn.1673-5374.2012.35.004
PMC:
PMID:
Suprachoroidal injection of ketorolac tromethamine does not cause retinal damage
Sumeng Liu1, Wu Liu2, Yaling Ma1, Kegao Liu2, Meizi Wang2
Rabbit right eyes were injected with 3 or 6 mg ketorolac tromethamine into the suprachoroidal space. Electroretinography results demonstrated no abnormal changes in rod cell response, maximum rod cell or cone cell mixing reaction, oscillation potential, cone cell response, waveform, amplitude, and potential of 30 Hz scintillation response in right eyes before injection, and at 1, 2, and 4 weeks after injection. There was no difference between left (control) and right eyes. Under light microscopy, the histomorphology of cells in each retinal layer was normal at 4 weeks following 6 mg ketorolac tromethamine administration. These results indicate that a single suprachoroidal injection of 3 or 6 mg ketorolac tromethamine into rabbits was safe. Suprachoroidal space injection appears to be safe.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#神经节细胞#
35
#酮咯酸#
32
#脉络膜#
29
#Res.:#
24