JAMA Oncol:EGFR抗体偶联药物MRG003治疗实体肿瘤的安全性和活性
2022-06-13 MedSci原创 MedSci原创
MRG003在EGFR阳性的鼻咽癌和头颈部鳞状细胞癌患者中表现出可控的安全性和有希望的抗肿瘤活性。
抗体药物偶联药物MRG003包含抗表皮生长因子受体 (EGFR) 人源化免疫球蛋白G1单克隆抗体,通过缬氨酸-瓜氨酸连接剂将该抗体与单甲基auristatin E偶联。目前尚无充足的证据证明该药物的安全性和有效性。
本研究旨在明确MRG003的最大耐受剂量,评估其安全性,同时探索其在EGFR表达患者中的初始抗肿瘤活性。
这是一项在我国开展的非随机、多中心、开放标签的单臂1期试验,分为两个部分:1a剂量递增期和1b剂量扩展期。1a期招募了不能接受标准治疗或治疗失败的晚期或转移性实体瘤患者(不考虑EGFR表达状态)。1b期招募EGFR阳性的难治性晚期头颈部鳞状细胞癌(SCCHN)、鼻咽癌(NPC)和结直肠(CRC)患者。在1a期,每3周予以一剂MRG003(0.1-2.5 mg/kg)。在1b期,予以1a期明确的推荐剂量。主要终点是1a阶段的剂量限制性毒性和1b期的客观缓解率。
不良反应发生情况
2018年4月11日-2021年3月29日期间,1a期招募了22位患者(平均54.5岁,9位女性),1b期招募了39位患者(平均50.4岁,8位女性)。推荐剂量定为2.5 mg/kg。89%的不良事件(AE)与MRG003治疗相关,大部分AE是1-2级的。19位(31%)患者报告了3级及以上的AE,包括低钠血症、白细胞减少症、中性粒细胞减少症、谷草转氨酶升高和发热性中性粒细胞减少症。
1b期所有患者的治疗反应
在1a期,1位(5%)患者获得了部分缓解,5位(23%)患者的病情保持稳定。在1b期,8位(21%)患者获得了部分缓解,12位(31%)患者的病情保持稳定。SCCHN、NPC和CRC患者的缓解率分别是40%、44%和0%,疾病控制率分别是100%、89%和25%。
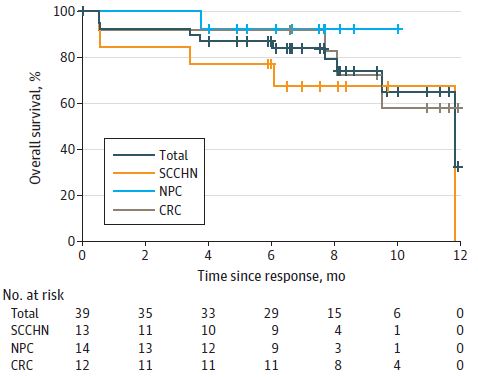
不同肿瘤患者的总生存率
综上,该研究结果显示,MRG003在EGFR阳性的鼻咽癌和头颈部鳞状细胞癌患者中表现出可控的安全性和有希望的抗肿瘤活性。
原始出处:
Qiu M, Zhang Y, Guo Y, et al. Evaluation of Safety of Treatment With Anti–Epidermal Growth Factor Receptor Antibody Drug Conjugate MRG003 in Patients With Advanced Solid Tumors: A Phase 1 Nonrandomized Clinical Trial. JAMA Oncol. Published online May 05, 2022. doi:10.1001/jamaoncol.2022.0503.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#Oncol#
36
学习了
55
不错,学习了。
40
#实体肿瘤#
45
#GFR#
52
JAMA上文章都是顶级的,谢谢梅斯及时上新
32