SABCS 2013:三阴性乳腺癌新辅助化疗获益
2013-12-27 MedSci MedSci原创
越来越多的三阴性乳腺癌患者在手术前接受新辅助化疗。大约有三分之一的患者,在新辅助化疗实施后,手术时乳腺组织中没有可识别的癌细胞并且淋巴结没有转移,也就是说这些患者出现病理完全缓解(pCR),并且与那些对新辅助化疗没有很好效果的患者相比癌症复发风险低的多。将化疗药物卡铂和/或者靶向治疗药贝伐珠单抗加入到标准术前化疗中,会使手术过程没有残留癌的三阴性乳腺癌患者的数量增加,这是公布在2013年圣安东尼奥
越来越多的三阴性乳腺癌患者在手术前接受新辅助化疗。大约有三分之一的患者,在新辅助化疗实施后,手术时乳腺组织中没有可识别的癌细胞并且淋巴结没有转移,也就是说这些患者出现病理完全缓解(pCR),并且与那些对新辅助化疗没有很好效果的患者相比癌症复发风险低的多。
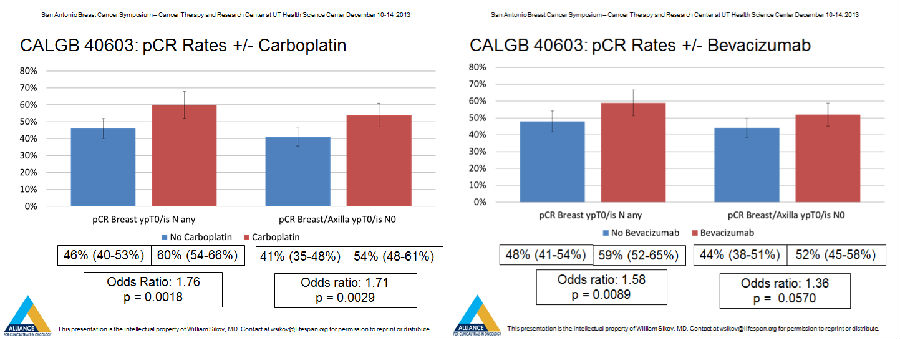
将化疗药物卡铂和/或者靶向治疗药贝伐珠单抗加入到标准术前化疗中,会使手术过程没有残留癌的三阴性乳腺癌患者的数量增加,这是公布在2013年圣安东尼奥乳癌研讨会上一项随机的,II期临床试验结果。
“我们研究的目的是确定增加卡铂或者贝伐珠单抗到标准术前化疗是否会增加手术前癌消除患者比例,很高兴的向大家报告,无论加入哪一种治疗都会显著地提高乳腺中癌消除患者的比例,并且这两种治疗的添加会更有效。”
“虽然我们的结果表明使用卡铂和贝伐珠单抗会增加病理完全缓解率,但我们还不知道影响到底有多大,如果有的话,这些差异将会表现在癌症复发或死亡方面。尽管这 项研究不足以大到可以检测这些终点的显著差异,我们计划在手术后随访患者10年去观察患者治疗效果显示的来自研究性治疗长期受益情况。”

布朗大学 Warren Alpert医学院的William M.Sikov教授根据这项随机的,II期临床试验研究发表了上述的观点。
该项研究是由Cancer and Leukemia Group B指导的,它是目前Alliance for Clinical Trials in Oncology的一部分,被称为CALGB/Alliance 40603。
Sikov和他的同事们在这项随机的,II期临床试验中,治疗了443例可手术的、2级或者3级三阴性乳腺癌患者。患者被随机分为标准新辅助化疗,标准新辅助化疗+卡铂,标准新辅助化疗+贝伐珠单抗和标准新辅助化疗+卡铂+贝伐珠单抗四组。手术治疗是在新辅助治疗完成四到八周后进行。
研究人员发现, 被随机分配到新辅助化疗组的108名患者中,手术时,乳腺肿瘤清除的比例是42%,乳腺和淋巴结都清除的比例是39%;对于随机分配到新辅助化疗+贝伐珠 单抗组中110名患者来说,这些比例分别提高到了50%和43%;随机分配到新辅助化疗+卡铂的113名患者,比例分别为53%和49%;随机分配到新辅 助化疗+卡铂+贝伐珠单抗组的112名患者,分别为67%和60%。
在随机分配到新辅助化疗+卡铂组的患者中,观察到乳腺以及乳腺和淋巴结的病理完全缓解率增加均具有统计学显著。而随机分配到新辅助化疗+贝伐珠单抗的患者中,只有乳腺的病例完全缓解率增加满足研究标准的显著性。
使用卡铂治疗对比没有接受卡铂的患者,会有更多关于血细胞计数降低的问题,并且有可能错过化疗、推迟化疗给药或者化疗药物剂量减少。另外,大约10%接受贝伐珠单抗治疗的患者会出现高血压,并且这些患者中更多的会出现血块、出血和感染的问题。
该项II期临床试验研究的只要内容请参看下文:
结果:454名患者参加此次研究,中位年龄是48岁,2级68%/3级32%。354名患者提供了治疗数据,59名患者没有完成新辅助化疗,20名患者由于不良反应退出试验。
通常由贝伐珠单抗引起与贝伐珠单抗无关的不良反应比例为11.5%和3.5%。随机分配的患者中使用贝伐珠单抗而终止治疗占23%,使用其它药物终止治疗的比例是6-13%。使用卡铂对比不用卡铂更常见3-4级中性粒细胞减少症和血小板减少症比例为56% vs 20%和22% vs 4%,而使用贝伐珠单抗对比不使用贝伐珠单抗引起高血压的比例为11% vs <1%。患者接受卡铂和贝伐珠单抗两种药物易见发热性中性粒细胞减少症,对比其他药物分别为19%和<7%。
在最初396例患者未经审核的结果中,没有证据表明卡铂和贝伐珠单抗的效果之间有相互作用,P(乳腺)=0.64和P(乳腺/腋窝)P=0.44。
结论:初步结果表明,卡铂或者贝伐珠单抗加入标准新辅助化疗中会增加II到III级三阴性乳腺癌患者的pCR率。接受这两种添加患者的pCR(乳腺)为60.6%,pCR(乳腺/腋窝)为50%。患者将会被随访RFS/OS以评估pCR在这些点的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ABC#
43
#阴性乳腺癌#
37
#新辅助#
33
#三阴性#
28
#SABCS#
46