Front Oncol:在抗EGFR联合同期放疗的基础上增加同期化疗可明显改善II-IVb期鼻咽癌患者预后
2021-12-21 yd2015 MedSci原创
研究表明,在抗EGFR联合同期放疗的基础上增加同期化疗可明显改善II-IVb期鼻咽癌患者预后。
鼻咽癌(NPC)是在我国南方比较常见,未分化型鼻咽癌是最常见的类型。近年来,放疗联合化疗已成为治疗的标准。常用的放疗技术为适形调强放疗(IMRT)。由于同期放化疗的某些毒性作用,同期放疗联合抗EGFR治疗目前也越来越广泛应用。2020年版鼻咽癌CSCO指南也进行推荐同期放疗联合抗EGFR治疗单药或化疗。但是目前没有大型研究比较两种策略的疗效。因此,来自中山大学肿瘤防治中心的团队开展了相关研究,比较在II-IVb期鼻咽癌患者中,IMRT+抗EGFR+顺铂对比IMRT+抗EGFR的疗效和安全性。相关结果发表在Frontiers in Oncology杂志上。
2011年1月-2015年11月,共有656例II-IVb期鼻咽癌患者同时接受抗EGFR联合IMRT治疗。首先,通过匹配潜在的预后因素,构建含302名患者的匹配队列。此外,对所有656例II-IVb期鼻咽癌患者进行了总生存期(OS)、无进展生存期(PFS)、局部无复发生存期(LRRFS)和远端无转移生存期(DMFS)的单因素和多因素分析,以确定预后因素,并通过匹配队列来确认结果。
302例匹配队列患者中,所有患者均接受西妥昔单抗(CTX)或尼妥珠单抗单抗(NTX)治疗,大多数患者(96.0%)每周接受CTX或NTX治疗,共5-8周期,并同时进行放疗治疗。抗EGFR+放疗(Target-RT)组和顺铂(CDDP)+ Target-RT组均为151例。
在Target-RT组中,患者中位年龄为50岁(范围18 - 74),80.1%的患者为男性。27.2%的患者为IV期, 67例(44.4%)患者治疗前血浆EBV DNA拷贝数大于4000拷贝/mL。尼妥珠单抗单抗(NTX)的使用比例(124/151,82.1%)高于西妥昔单抗(CTX) (27/151,17.9%)。
在CDDP + Target-RT组中,患者中位年龄为49岁(范围10-72),81.5%的患者为男性。31.8%的患者为IV期,77/151(51.0%)患者的治疗前血浆EBV DNA拷贝数大于4000拷贝/mL。尼妥珠单抗单抗(NTX)的使用比例(113/151,74.8%)高于西妥昔单抗(CTX) (38/ 151, 25.2%)。
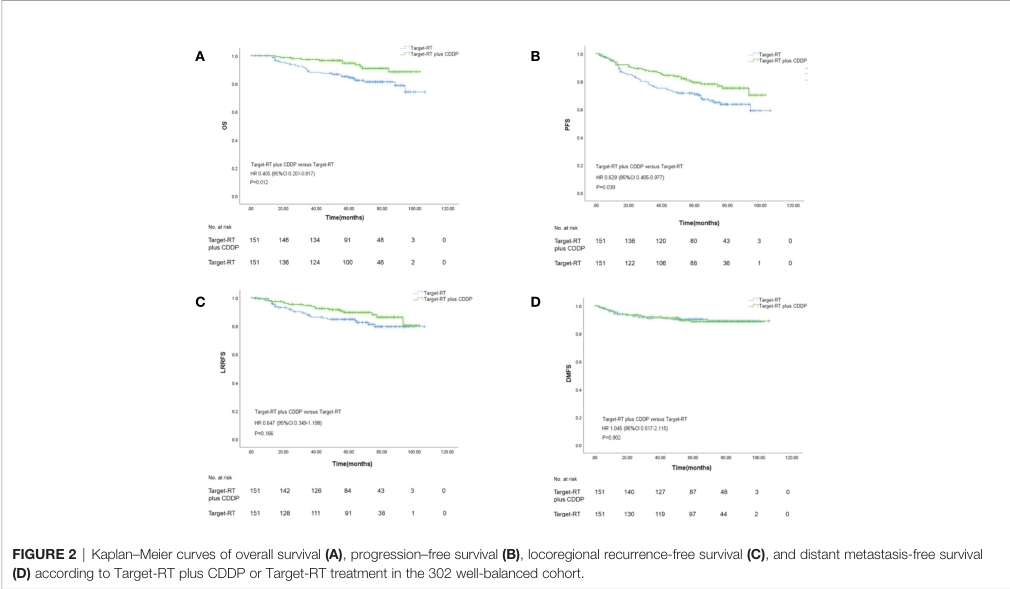
最后一次随访时间为2020年10月,中位随访时间为67.5个月(95%可信区间(CI): 66.1-68.9个月)。研究报告了38例死亡(Target-RT组27例,CDDP + Target-RT组11例)。共报告83例疾病进展,其中Target-RT组50例,CDDP + Target-RT组33例。Target-RT + CDDP组和Target-RT组5年OS率分别为94.7%和84.3% (P=0.012)。在PFS方面,Target-RT + CDDP组和Target-RT组的5年PFS率分别为82.0%和71.7% (P=0.039)。LRRFS和DMFS的分析未显示CDDP对生存结果的显著疗效。Target-RT + CDDP组和Target-RT组的5年LRRFS率分别为89.6%和84.8% (P=0.166), Target-RT + CDDP组和Target-RT组的5年DMFS率分别为88.6%和90.3% (P=0.902)。
预后分析
Target-RT + CDDP组出现3 - 4级血液学毒性的患者更多(40.4% vs 19.8% P<0.001),尤其是白细胞减少(31.8% vs 15.2%, P=0.001)。此外,Target-RT + CDDP组比Target-RT组发现更多的3-4级黏膜炎(28.5% vs 13.2% P=0.001)。
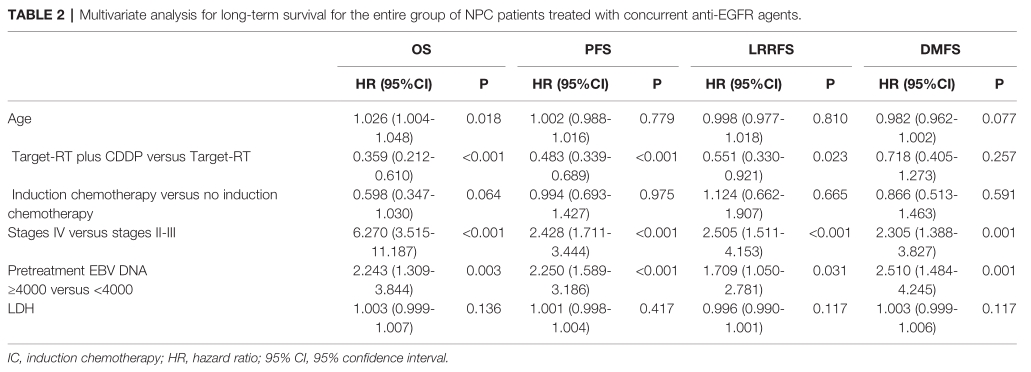
多因素分析发现,Target-RT + CDDP对比Target-RT治疗是OS(HR=0.359,95%CI 0.212-0.610,P<0.001),PFS(HR=0.483, 95%CI 0.339-0.689,p<0.001)和LRRFS(HR=0.551, 95%CI 0.330-0.921,p=0.023)的独立预后因素。
预后多因素分析
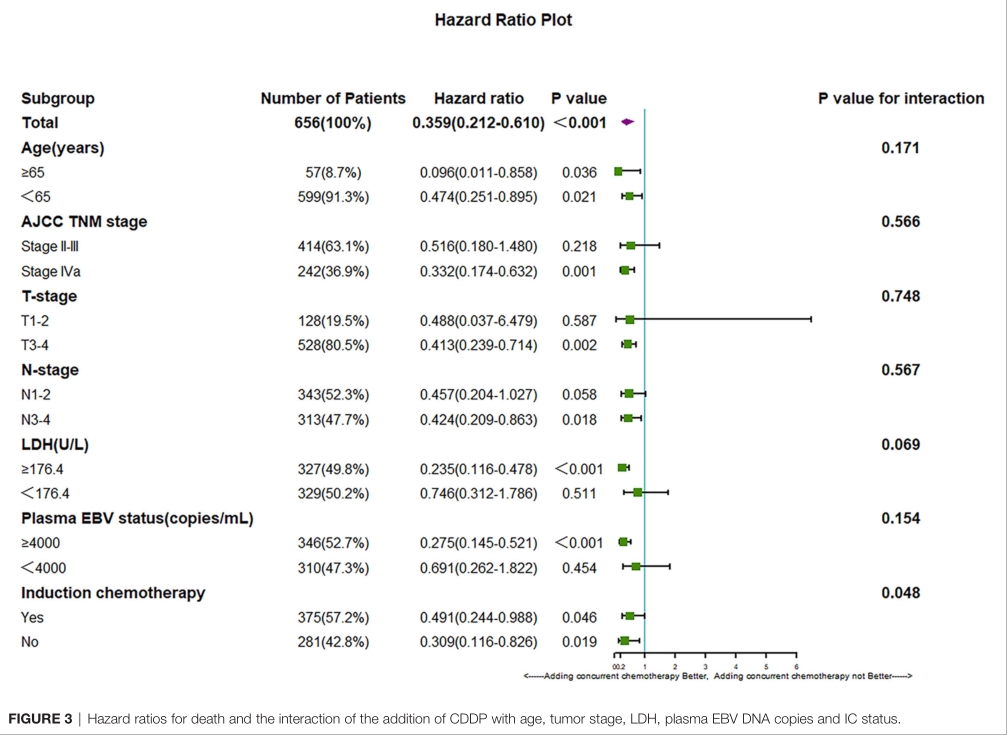
亚组分析发现,增加顺铂化疗可改善全年龄、IVa期、T3-4期、N3-4期、LDH≤176.4U/L、血清EBV≥400 coples/mL、伴或不伴诱导化疗等亚组患者的预后。
亚组分析
综上,研究表明,在抗EGFR联合同期放疗的基础上增加同期化疗可明显改善II-IVb期鼻咽癌患者预后。
原始出处:
Yu Z-K, Chen X-Y, Liu S-H, Liu Y-P, You R and Huang P-Y (2021) Adding Concurrent Chemotherapy Significantly Improves the Survival of Stage II-IVb Nasopharyngeal Carcinoma Patients Treated With Concurrent Anti-EGFR Agents. Front. Oncol. 11:814881. doi: 10.3389/fonc.2021.814881.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#患者预后#
41
#同期#
52
#Oncol#
0
#GFR#
35