JAMA Pediatrics:产前诊断胎儿是否患有先心病与有助于降低其脑损伤发生率
2016-02-29 QQduhp 译 MedSci原创
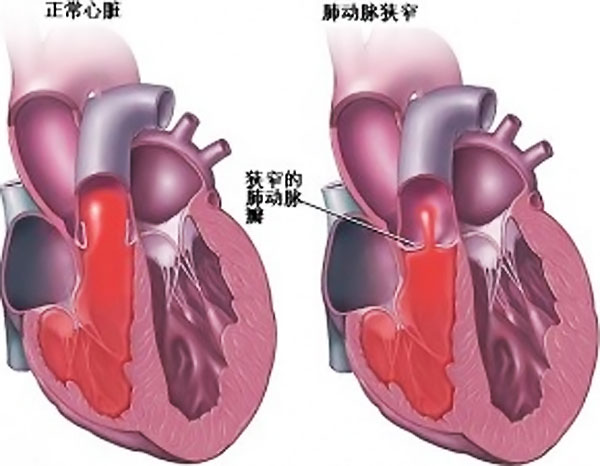
研究人员指出,产前诊断患有先天性心脏病(CHD)的新生儿相比产后诊断CHD的新生儿患脑损伤的发生率更低。产前检测胎儿是否患有CHD有助于改善新生儿围手术期的心血管状况,但大家并不知道这一诊断与新生儿脑损伤的关系。 加州大学的Shabnam Peyvandi博士和他的同事比较153名患有大动脉转位(TGA)和单心室 (SVP)的患儿术前和术后脑损伤的患病率。其中67名婴儿产前诊断患有CHD,而其余8
研究人员指出,产前诊断患有先天性心脏病(CHD)的新生儿比产后诊断CHD的新生儿患脑损伤的发生率更低。产前检测胎儿是否患有CHD有助于改善新生儿围手术期的心血管状况,但大家并不知道这一诊断与新生儿脑损伤的关系。
加州大学的Shabnam Peyvandi博士和他的同事比较153名患有大动脉转位(TGA)和单心室 (SVP)的患儿术前和术后脑损伤的患病率。其中67名婴儿产前诊断患有CHD,而其余86名患儿没有。
研究人员发现,产前诊断胎儿患有CHD后,婴儿术前出现脑损伤的患病率是24%,产后诊断新生儿患有CHD后,婴儿出现术前脑损伤的发生率为48%(p=0.003),在产前及产后诊断CHD的婴儿术后脑损伤的患病率相似。该研究结果发表在JAMA Pediatrics。
相比产后诊断CHD的患儿而言,产前诊断CHD的患儿大脑发育更快,术前和术后MR对照发现,产前诊断CHD的患儿大脑灰质的增长速度提高50%,白质的增长速度可提高70%。这可能是由于早发现,然后早期使用前列腺素E1进而导致患儿的血流动力学状态更好恢复。然而,研究人员仍需进一步探索遗传倾向、术中损伤或术后血流动力学等因素对患儿大脑的长期影响。他们表示还需要进一步的研究来确定是否进行产前诊断,以减少患儿术前脑损伤和改善大脑发育,可使儿童的大脑神经发育更好。
埃默里大学Matt Oster博士指出,产前检出率可能有助于减少CHD患儿的脑损伤发生率,但仍有约1/4的孩子会出现脑损伤。尽管早期诊断胎儿是否患有先天性心脏病有助于使婴儿的病情更加稳定,并为其争取进行手术的时间,但他们的长期生存率并不乐观,因为患有CHD的婴儿极易发生感染,这会为他们带来致命威胁。
原始出处:
Prenatal Diagnosis of Critical Congenital Heart Disease Tied to Less Brain Injury,Medscape. Feb 26, 2016.
Peyvandi S, De Santiago V,et al.Association of Prenatal Diagnosis of Critical Congenital Heart Disease With Postnatal Brain Development and the Risk of Brain Injury.JAMA Pediatr. 2016 Feb 22.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
30
#Pediatric#
28
#发生率#
26
#DIA#
34
#先心病#
27
#损伤#
27
#产前诊断#
28
#产前#
32
这个厉害饿
105