JAMA:华法林可改善伴房颤的急性心梗患者预后
2014-03-07 高晓方 译 医学论坛网
瑞典一项研究表明,在伴有房颤的急性心梗患者中,华法林治疗与死亡、心梗和缺血性卒中复合转归风险降低具有相关性,并且未升高出血风险。论文3月5日在线发表于《美国医学会杂志》。 此项研究共纳入24317例血清肌酐水平已知且伴有房颤的急性心梗存活者,并且21.8%的受试者在出院时应用华法林。依据估计肾小球滤过率(eGFR)对慢性肾病分级加以归类。复合终点由死亡以及心梗或缺血性卒中再次住院组成。主要转归指
瑞典一项研究表明,在伴有房颤的急性心梗患者中,华法林治疗与死亡、心梗和缺血性卒中复合转归风险降低具有相关性,并且未升高出血风险。论文3月5日在线发表于《美国医学会杂志》。
此项研究共纳入24317例血清肌酐水平已知且伴有房颤的急性心梗存活者,并且21.8%的受试者在出院时应用华法林。依据估计肾小球滤过率(eGFR)对慢性肾病分级加以归类。复合终点由死亡以及心梗或缺血性卒中再次住院组成。主要转归指标为复合终点、出血以及二者综合。
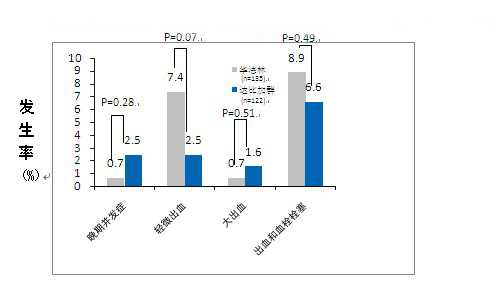
结果显示,共有5292例患者在出院时应用华法林,其中51.7%伴有明显慢性肾病(eGFR<60 mL/min/1.73 m2)。与未应用华法林相比,在各慢性肾病分层中华法林应用均与复合终点风险降低具有相关性。在各慢性肾病分层中,华法林治疗者的出血风险出现非显著升高。华法林应用与综合转归出现风险降低具有相关性。
原始出处:
Juan Jesús Carrero, PhD(Pharm and Med)1,2; Marie Evans, MD, PhD2; Karolina Szummer, MD, PhD3; Jonas Spaak, MD, PhD4; Lars Lindhagen, PhD5; Robert Edfors, MD3; Peter Stenvinkel, MD, PhD2; Stefan H Jacobson, MD, PhD4; Tomas Jernberg, MD, PhD3.Warfarin, Kidney Dysfunction, and Outcomes Following Acute Myocardial Infarction in Patients With Atrial Fibrillation.JAMA. 2014;311(9):919-928. doi:10.1001/jama.2014.1334.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心梗患者#
26
#患者预后#
37
#急性心梗#
29
内容不错。
130