WCLC速递:拨云见日,未来可期:数据证实奥希替尼在继发T790M耐药和脑转移患者中疗效确切
2018-09-30 佚名 肿瘤资讯
世界肺癌大会(World Conference on Lung Cancer,WCLC)是全球最大的致力于肺癌和其他胸部恶性肿瘤的学术会议,也是唯一一个致力于肺癌研究的全球性组织。大会每年一度,2018年WCLC在当地时间9月23日于秋日风景如画的多伦多拉开序幕。今年WCLC会议的主题是“Take action against lung cancer!” 靶向治疗仍然是肺癌研究中的重要议题。201
奥希替尼治疗EGFR T790M阳性NSCLC的真实世界数据
MA02.03. ASTRIS研究:奥希替尼治疗EGFR T790M阳性患者的真实世界研究
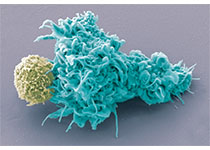
奥希替尼是第三代、有CNS活性的 EGFR-TKI,可以高效的、选择性的抑制EGFR敏感突变和T790M耐药突变。ASTRIS 研究是一项全球研究,也是目前最大样本量的评估奥希替尼用于真实世界的临床研究。本研究评估奥希替尼治疗既往接受过EGFR TKI治疗后T790M突变阳性NSCLC患者的疗效和安全性。这一研究同时特别关注奥希替尼治疗特定人群的疗效:PS 2分,年龄75岁或以上以及合并罕见EGFR突变的患者。
研究入组标准为局部晚期或转移性NSCLC,WHO PS 0-2分,T790M阳性,既往接受过至少一线EGFR TKI治疗,允许无症状脑转移患者入组。患者接受奥希替尼80 mg/天。主要研究终点为OS,次要终点包括临床缓解率、PFS、至治疗中止时间、安全性和耐受性。2015年9月18日至2017年10月10日,研究从16个国家入组了 3014例至少接受过≥1个剂量奥希替尼治疗的患者(纳入全分析集 [FAS])。入组患者的中位年龄为62岁(27–92),64%为女性,69%为亚裔,WHO PS 评分0/1/2分的患者分别占26%/63%/11%。合并罕见或复杂EGFR突变的患者占4%。所有患者均为 T790M阳性,其中1611例(53%)患者经组织标本检测;1241例(41%)经血浆ctDNA检测,162例(5%)经其他标本检测。
至数据截止日期的中位随访时间为 7.9 个月(范围<1?24)。1276例(42%)患者中止治疗,1738例患者 [58%] 仍在接受治疗。中位治疗时间为 7.4 个月 (范围:<1–25个月);593 例(20%) 患者死亡。在 FAS集中,预计的中位PFS为11.0个月(95% CI 10.6, 11.1)。
总人群的临床缓解率为56.1% (1611/2870*; 95% CI 54.3, 58.0)。中位TTD 为12.6个月(95% CI 12.2, 13.7),中位OS 尚未达到(12个月的OS 率为75.8% (95% CI 73.7, 77.8)。亚组分析显示,年龄≥75岁、EGFR罕见突变的患者,接受奥希替尼治疗的mPFS与总体人群相当。WHO PS 2分的患者对比PS 0-1分的患者,mPFS分别为6.9 vs 11.1个月。(*144名患者截止分析时有效率无法评估)
安全性分析显示,任意级别的不良事件(AE)发生率为24%。因AE导致剂量调整和治疗中止的患者比例分别为11%和5%。间质性肺炎/类肺炎事件发生率为1% ,QT间期延长发生率为2%。15例(<1%)患者出现≥3度ILD或类肺炎事件。无患者因为QT间期延长危及生命。
结论
在这一大型、全球的真实世界研究中,奥希替尼的疗效和安全性与AURA系列研究数据一致。亚组分析显示,在EGFR罕见或复发突变(对比常见突变)或年龄≥75岁(<75岁)的患者中,奥希替尼显示出一致的疗效。这一研究同时发现在PS2分的患者中,奥希替尼同样显示出临床获益。ASTRIS研究是目前最大样本量的评估奥希替尼治疗T790M阳性的NSCLC患者的研究,观察到与临床试验相似的临床疗效,且未出现新的安全性事件。
奥希替尼对脑转移患者同样安全有效
P1.13-25. APOLLO研究:奥希替尼治疗中国EGFR T790M阳性伴脑转移晚期NSCLC患者的有效性和安全性
在AURA系列研究中已经证实奥希替尼在中枢神经系统(CNS)转移的一代TKI耐药T790M阳性NSCLC患者中具有良好的有效性,但在中国患者中的疗效数据有限。本研究旨在评估奥希替尼在用于合并CNS转移T790M阳性患者的有效性和安全性,并使用配对脑脊液(CSF)和血浆样本探讨其潜在机制。这是一项单臂多中心前瞻性研究。入组已经接受过一代EGFR TKI治疗进展后T790M阳性并伴有脑转移的晚期NSCLC。患者接受奥希替尼80mg qd治疗直至进展。主要终点为总体人群的PFS(PFSo);次要终点包括颅外PFS(PFSe)、颅内PFS(PFSi)、ORR、DCR、DOR、安全性和OS。分别在基线、治疗后6周和疾病进展时收集成对CSF-血浆样本,采用NGS进行分析。探索性终点包括配对样本中的动态基因变化,药物的血脑屏障穿透率。38例符合条件的患者入组,其中12例收集了配对CSF-血浆样本。基线的特征总结见下表1。
主要研究终点分析,中位PFSo(成熟度60%,23/38)为8.4个月(95% CI,5.8~11.0),中位PFSe和PFSi分别为10.2和10.9个月。总体人群的ORR为42.4%,颅外和颅内ORR分别位39.4%和71.9%。临床疗效总结见图2和表2。安全性分析显示,3级以上的AE发生率为39.5%。
对12个配对CSF-血浆样本进行分析,奥希替尼的中位CSF渗透率为31.7%(范围19.8~57.7),中位CSF浓度为10.8nM(范围5.2~30.3),见表3。基线时,分别在83%(10/12)的血浆样本和17%(2/12)的CSF样本检测到T790M突变,两者的一致率为8.3%(1/12),见表4。在治疗第6周时EGFR敏感性突变清除的患者,比持续检测到EGFR敏感突变的患者,中位PFSo现在更长,分别为未达到vs 2.83个月;HR 0.09;95% CI:0.02-0.54;P<0.01,见下图3。
该研究证实,在伴有脑转移的EGFR T790M阳性中国晚期NSCLC患者中,奥希替尼显示出卓越的疗效、良好的血脑屏障渗透性和可控的耐受性。NGS分析显示,血浆和CSF样本具有异质性,纵向动态进行基因分析可能有助于预测奥希替尼的疗效。
总结
AURA系列研究助力奥希替尼成为治疗T790M突变的全球唯一上市药物,而ASTRIS研究则在真实世界中再次夯实奥希替尼治疗T790M阳性NSCLC的疗效和安全性。在真实世界中组织标本检测仅占一半,液体活检已经成为T790M检测最重要的组成部分,目前来看,相比于血液检测,组织检测的敏感度依然有着不可动摇的优势,临床首选取材标本依然是肺癌组织;血液标本虽然具有可及性、取材便利性等特点,但敏感度不足一项无法让它的优先级与组织标本检测相平齐。研究的PFS为11个月,但TTD为12.6个月,也就是说,在疾病进展后奥希替尼仍继续使用了1.6个月,说明尽管进展,但临床上仍认为三代TKI可以使患者长期获益,APOLLO研究也初步证实了奥希替尼对于脑转移的疗效,可作为控制颅内病灶的治疗选择。真实世界中有11%患者因为毒性减量,而5%患者因为毒性被迫中断治疗,要进一步分析减量和中断治疗的原因。ASTRIS研究作为一项真实世界(RW)研究,相比传统的RCT能更贴近临床实际,这是RW研究独有的不可替代的优势,因此ASTRIS的研究成果能更好地被临床医生所接受和应用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#T790M耐药#
33
#脑转移患者#
37
#继发#
21
#T790M#
29
#WCLC#
33
学习了,谢谢作者分享!
63
谢谢梅斯提供这么好的信息,学到很多
50
了解一下,谢谢分享!
69