BMJ:结肠癌生存期预测影响因素
2017-07-11 zhangfan MedSci原创
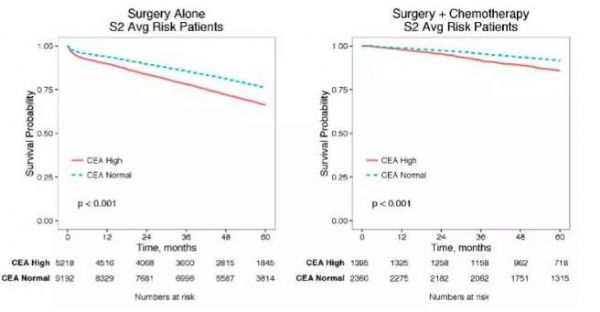
研究开发并验证了结直肠癌风险预测模型,以评估整体和有条件的与患者生存相关的临床和人口特征。该研究可以为患者提供更个性化的信息指导与结直肠癌治疗的后续决策
近日研究人员开发并外部验证了一种结直肠癌患者生存预测模型。共44145名,15-99岁的结肠癌患者参与了模型的推导过程,15214名患者参与了模型验证过程。研究的主要终点是全因死亡率,次要终点是结肠癌死亡。研究采取特定风险模型对直肠癌的死亡率和其他原因死亡率进行预测。性别为独立的推导因素,其他的影响因素包括:年龄,种族,能力丧失评分,肿瘤分期、肿瘤分级、手术、化疗、放疗、吸烟、饮酒、体重指数、肠癌家族史,贫血,肝功能,合并症,使用他汀类药物、阿司匹林、贫血和血小板计数。在模型推导后的第1,5,10年进行校准。最终的男女性模型包括以下变量:年龄,能力丧失评分、癌症分期、肿瘤分级、吸烟状态、结直肠手术,化疗,大肠癌家族史、血小板计数、肝功能异常、心血管疾病、糖尿病、慢性肾脏疾病、慢性阻塞性肺疾病,服用阿司匹林和他汀类药物。女性患者生存率提高的影响因素:年龄小、癌症早期、较好或中度的肿瘤分级、手术(相对风险 0.50), 结肠癌家族史 (0.62),服用他丁类药物 (0.77)和阿司匹林(0.83)。风险方程进行校准发现在验证队列中男性和女性的差异良好。研究开发并验证了结直肠癌风险预测模型,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
33
#生存期#
26
#影响因素#
25
谢谢分享,学习了
43
学习了,涨知识
67
签到学习了很多
49