BMJ:398个城市的多地点分析——环境NO2与每日总死亡率、心血管和呼吸系统疾病死亡率的短期相关性
2021-03-25 MedSci原创 MedSci原创
二氧化氮(NO2)是一种常见的空气污染物,对人群健康有不良影响,是地面臭氧的前体,自身对健康有不良影响,并参与细颗粒物的二次形成。大多数环境中的NO2都是人为的,比如燃料燃烧和交通。许多研究报告了短期
二氧化氮(NO2)是一种常见的空气污染物,对人群健康有不良影响,并参与细颗粒物的二次形成。大多数环境中的NO2都是由人类活动引起的,比如燃料燃烧和交通。许多研究报告了短期暴露于NO2对人类死亡率或发病率的影响,但这些都是有争议的。
美国环境保护署进行的综合科学评估审查了2008年和2016年NO2暴露与健康结果之间的现有证据,并得出结论,短期接触NO2与对呼吸的影响之间存在因果关系。而不同政府和政府间机构通过的空气质量准则中NO2的限制不同。

Pixabay.com
本研究旨在通过调查NO2与全球众多国家/地区死亡率之间的短期关联,利用来自多城市多国合作研究网络的数据来检验这些局限性(https://mccstudy.lshtm.ac.uk/)。该评估利用了一个最先进的流行病学方法的统一分析框架,以估计灵活的暴露反应关联,整合城市和国家的结果,并量化短期NO2暴露造成的超额死亡率。评估全球多个国家/地区NO2与总死亡率、心血管死亡率和呼吸死亡率之间的短期相关性。
本研究采用两阶段,时间序列方法,过度分散的广义线性模型和多层次元分析。研究包括来自22个低收入至高收入国家/地区的398个城市。主要研究结果测量:1973年至2018年间,每日死于总死因(6280万)、心血管原因(1970万)和呼吸原因(550万)的人数。
研究结果显示,平均而言,滞后1天(前一天)的NO2浓度增加10μg/m3分别与总死亡率、心血管死亡率和呼吸死亡率增加0.46%(95%置信区间0.36%至0.57%)、0.37%(0.22%至0.51%)和0.47%(0.21%至0.72%)相关。在调整了共污染物(空气动力学直径为10μm或2.5μm的颗粒物(分别为PM10和PM2.5)、臭氧、二氧化硫和一氧化碳)后,这些关联仍然很强。所有三种原因的混合浓度-反应曲线几乎呈线性,没有明显的阈值。在398个城市中,由于NO2浓度高于反事实零水平而导致的死亡比例为1.23%(95%置信区间为0.96%至1.51%)。

22个国家/地区398个城市的死亡率和环境数据
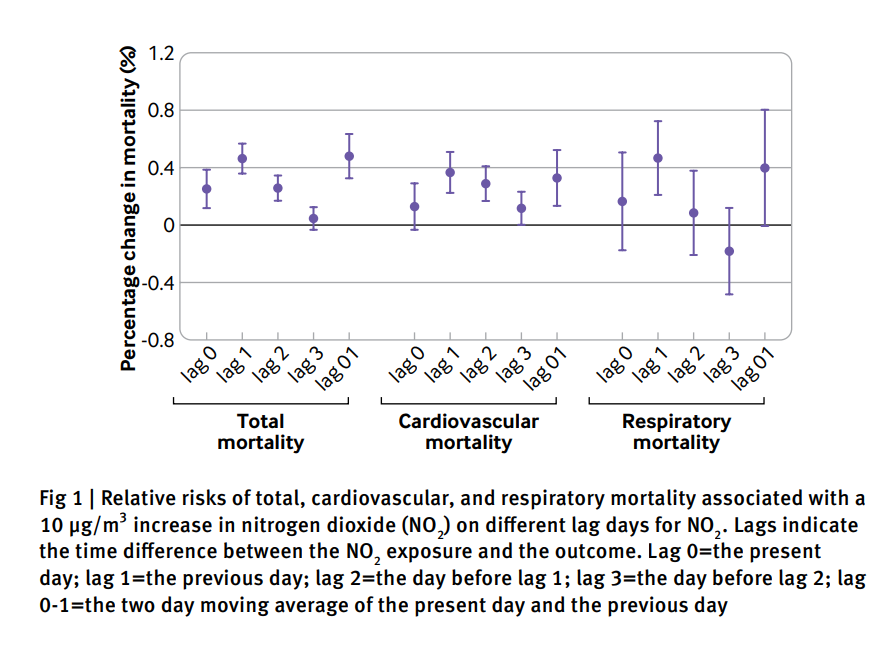
总死亡率、心血管死亡率和呼吸死亡率的相对风险与NO2在不同滞后天数内增加10 μg/m3 相关
这项关于二氧化氮与每日死亡率短期关联的流行病学研究的一个关键优势是使用相同的分析方案对大型数据集进行分析,这使得世界各国和地区之间能够进行有效的比较。本研究发现NO2与总死亡率、心血管疾病和呼吸系统疾病的日死亡率之间存在着密切的联系,而这与其他空气污染物的伴随暴露无关。更重要的是,研究者汇集了全球水平的NO2浓度响应曲线,表明二者几乎呈线性相关,没有可识别的阈值。这一结果表明,即使在低于以健康为基础的标准和准则(包括世卫组织目前的空气质量准则)的水平,二氧化氮也与相当大的健康风险有关。
总之,这种多地点时间序列分析为短期暴露于NO2与总死亡率、心血管死亡率和呼吸系统死亡率风险增加的独立关联提供了有力的证据,尽管由于研究地点没有完全覆盖全球,总死亡率负担可能被低估。浓度响应曲线呈线性,无明显阈值,表明需要修订和加强当前的NO2空气质量指南,以提高公众健康效益,并考虑对日平均NO2浓度的监管限制。这些发现有助于更好地了解如何优化公共卫生行动和战略,以减轻空气污染。
参考文献:Short term associations of ambient nitrogen dioxide with daily total, cardiovascular, and respiratory mortality: multilocation analysis in 398 cities BMJ 2021; 372 doi: https://doi.org/10.1136/bmj.n534 (Published 24 March 2021)Cite this as: BMJ 2021;372:n534
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#相关性#
32
#NO2#
27
#BMJ#
28
#呼吸系统疾病#
43
加油
71