JAMA Surg:疲劳、黄疸进行性加重5月,体重下降案例报道
2016-02-19 Mechront 译 MedSci原创
64岁男性,疲劳、黄疸进行性加重5月,体重下降13kg,否认发热、寒颤、腹痛。查血:总胆红素14.4 mg/dL,转氨轻度升高,白细胞 13 300/mL,血清癌胚抗原 1.9 ng/mL,肿瘤抗原 293 U/mL。CT:不均匀增强肝门肿块,伴广泛的肝内胆管扩张。肿块大小约 4.4 × 4.3 × 3.5 cm。胆囊钙化。肺部左上叶可见部分钙化结节,大小约7mm。心膈和胃淋巴结肿大。内镜下逆行胰
64岁男性,疲劳、黄疸进行性加重5月,体重下降13kg,否认发热、寒颤、腹痛。
查血:总胆红素14.4 mg/dL,转氨轻度升高,白细胞 13 300/mL,血清癌胚抗原 1.9 ng/mL,肿瘤抗原 293 U/mL。
CT:不均匀增强肝门肿块,伴广泛的肝内胆管扩张。肿块大小约 4.4 × 4.3 × 3.5 cm。胆囊钙化。肺部左上叶可见部分钙化结节,大小约7mm。横膈和胃淋巴结肿大。
胆管细胞学检查:反应性导管上皮细胞,无恶性肿瘤细胞。
内镜超声检查和细针抽吸:芽肿性变化,炎症细胞肉。
定量FERON、血清隐球菌抗原、血清荚膜组织胞浆菌抗原均阴性。CT引导下肝穿刺活检显示需氧、厌氧、分枝杆菌、真菌均阴性。
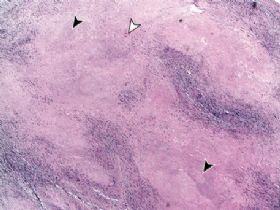
腹腔镜活检:巨型细胞坏死性肉芽肿性炎症和中央坏死。银银乌洛托品和抗酸染色:真菌和分枝杆菌阴性。
诊断:肝门部胆管癌(汇管区肿瘤)?肝结核?淋巴瘤样肉芽肿病?肝脏朗格汉斯细胞组织细胞增生症?
对患者的肿块组织病理学检查显示坏死性肉芽肿性炎症,提示结核分枝杆菌感染。虽然抗酸染色和分枝杆菌培养阴性,但两种检查方式的阳性率仅在0%-45%和10%-60%。就算是细针抽吸聚合酶链反应分析,其阳性预测值也只有57%。
原发性肝结核的很罕见,常见于旧的肺结核复发所致。患者的流行病学史,结合胸部CT表现,可对其进行诊断。
查血结果、梗阻性黄疸表现、影像学资料等提示肝门部胆管癌的可能,但是细针穿刺检查和腹腔镜肝活检均没有发现肿瘤的证据。
坏死性肉芽肿性肝炎的鉴别诊断包括感染、自身免疫性疾病、药物反应和淋巴瘤样肉芽肿病。肺部常见,肝脏病变的报道占29%。朗格罕细胞组织细胞增生症的典型特点是肺、骨、淋巴结和皮肤的肉芽肿性炎症,≥55岁的患者中只有10%的诊断率。
结合临床、影像学、病理结果排除肿瘤、血管炎、免疫疾病,可疑肝结核,临床抗结核治疗效果好,证实患者肝结核的诊断。抗结核治疗的临床反应通常出现在开始治疗后的2至3个月。
如果结核压迫相关胆道导致黄疸、门静脉高压症、胆道出血或诊断不明时,可能会需要手术干预。
原始出处:
Steve M. Niemiec,Joseph M. Vinetz, et al.Porta Hepatis Mass.JAMA Surg. 2016;151(2):187-188.doi:10.1001/jamasurg.2015.2425.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











很少见学习了
133
很好,谢谢啦
93
学习习
112
少见
135
#进行性#
37
#疲劳#
32
#黄疸#
32
很少见,不说完全想不到
111
有用
73