AACR 2022:第四代EGFR抑制剂BLU-945治疗晚期耐药的NSCLC早期结果公布
2022-04-11 网络 网络
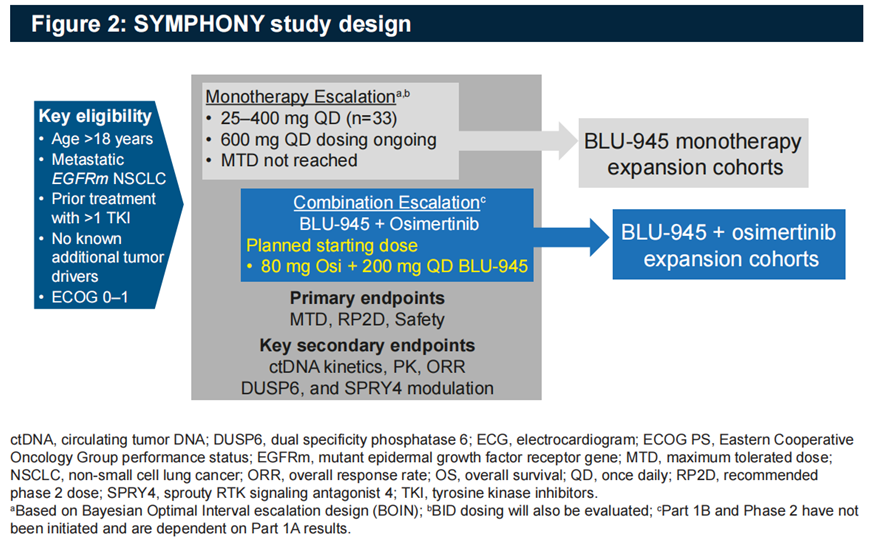
SYMPHONY(NCT04862780)研究是BLU-945的首次人体1/2期开放性标签临床试验,旨在评估BLU-945单药和联合奥希替尼治疗对EGFR-TKI耐药的晚期NSCLC患者的安全性、耐受
SYMPHONY(NCT04862780)研究是BLU-945的首次人体1/2期开放性标签临床试验,旨在评估BLU-945单药和联合奥希替尼治疗对EGFR-TKI耐药的晚期NSCLC患者的安全性、耐受性和有效性。
BLU-945是BluePrint公司的新一代产品,目前正在开展多项临床试验。

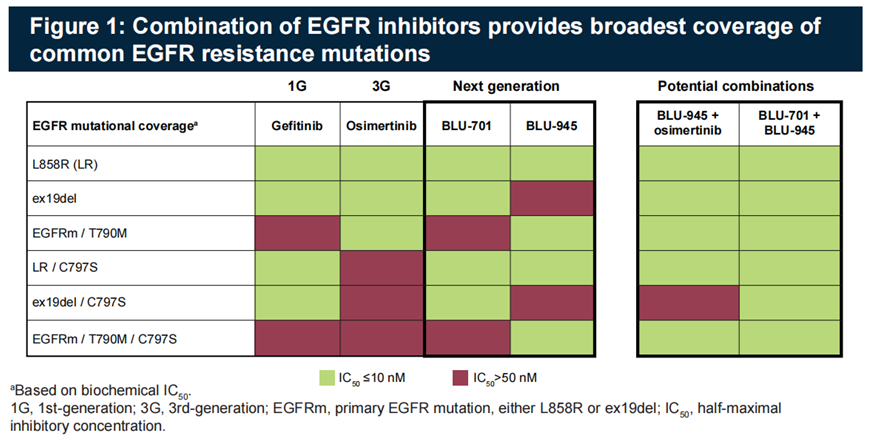
临床前数据显示,BLU-945对EGFR L858R,L858R/T790M,Del 19/T790M,L858R/C797S,L858R/T790M/C797S,Del/T790M/C797S高度敏感,而联合奥希替尼或BLU-701可以增强对Del19和Del19/C797S突变的效力,见图1。
SYMPHONY(NCT04862780)研究临床设计方案见图2。
※患者基线特征
剂量爬坡阶段,截至2022年3月9日,5个队列共33例EGFR突变晚期NSCLC患者接受了BLU-945单药25mg-400mg每天一次的治疗。
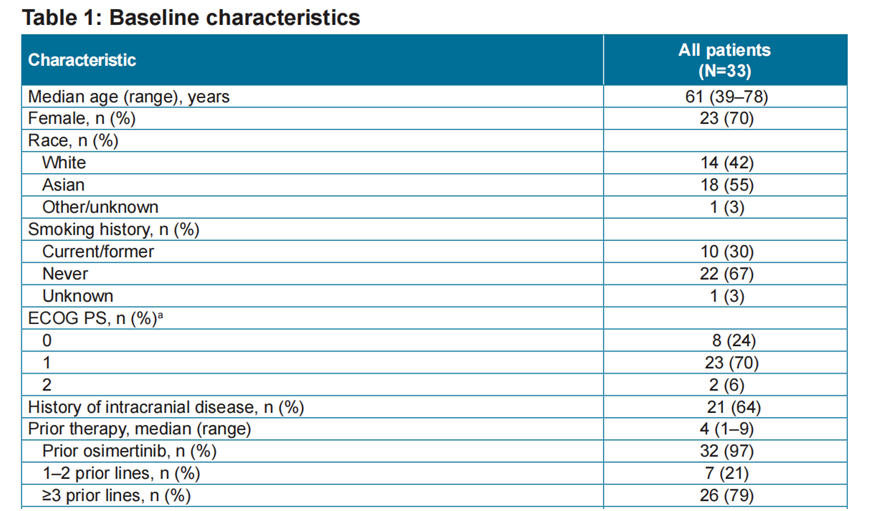
患者的中位年龄61岁,70%女性,42%白人,55%亚洲人,67%无吸烟史,94%PS 0-1分,64%脑转移,97%使用过奥希替尼,79%已经历了三线以上治疗。
BLU-945第一个疗程的第1天,用FoundationOne液体活检平台检测了患者的外周血中游离DNA,其中4例无数据,8例EGFR突变未检出,1例仅T790M,6例仅L858或Del 19,1例L858或Del 19/C797S,1例L858或Del 19/T790M,11例(33%)C797S三联突变。
※临床结果
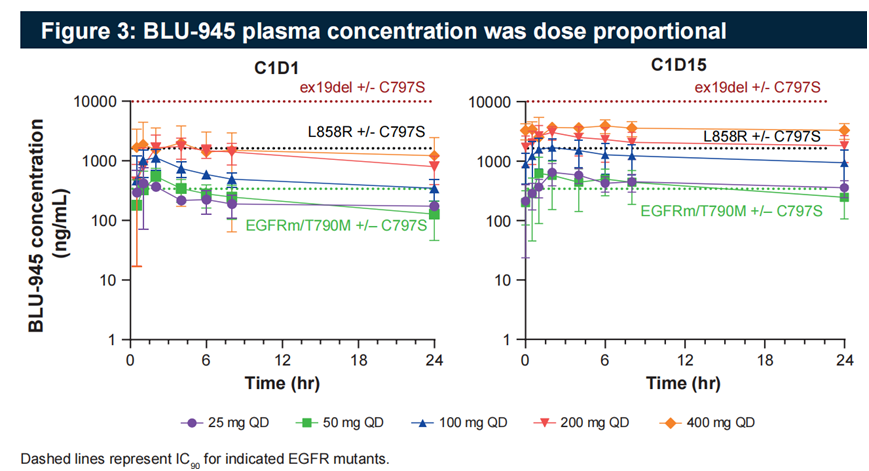
BLU-945的平均半衰期为24.1小时,其血药浓度与剂量成正比。
BLU-945第一个疗程的第15天和第1天的外周血中游离DNA含量比较结果见图4。
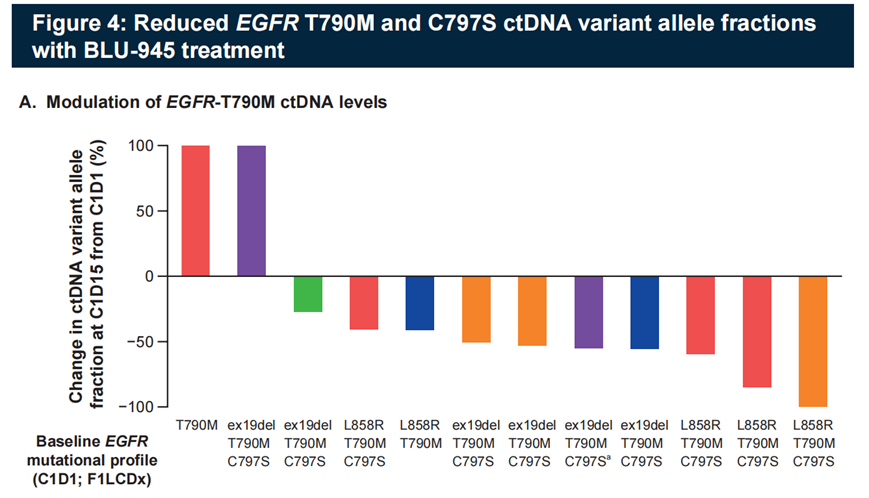
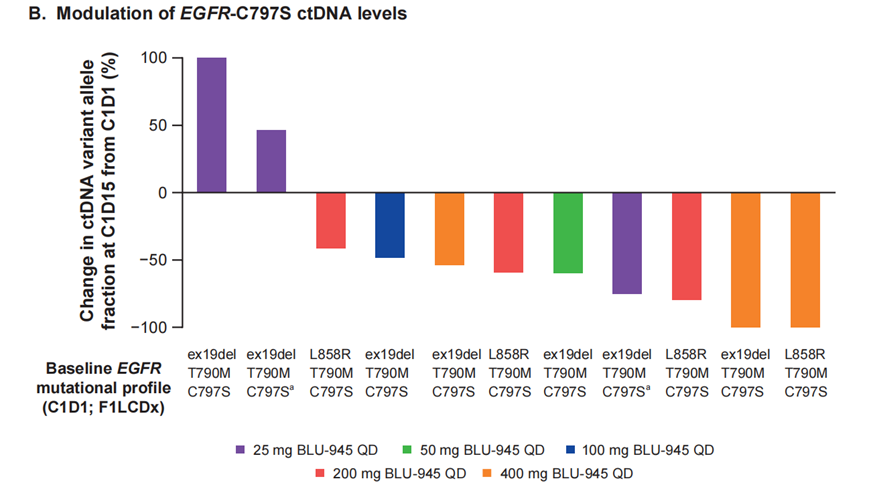

包括所有剂量水平时,81%的C797S含量在BLU-945第15天时出现下降,而400mg剂量水平时,所有患者的T790M和C797S水平都出现下降,其中3例患者降至未检出。
BLU-945的抗肿瘤效力和剂量成正比,在 200mg每天一次以上的剂量水平时,观察到肿瘤缩小,包括1例未确认的部分缓解,见图5。2例患者在100mg每天一次时,肿瘤增大,加量至200mg每天一次后,肿瘤出现缩小。

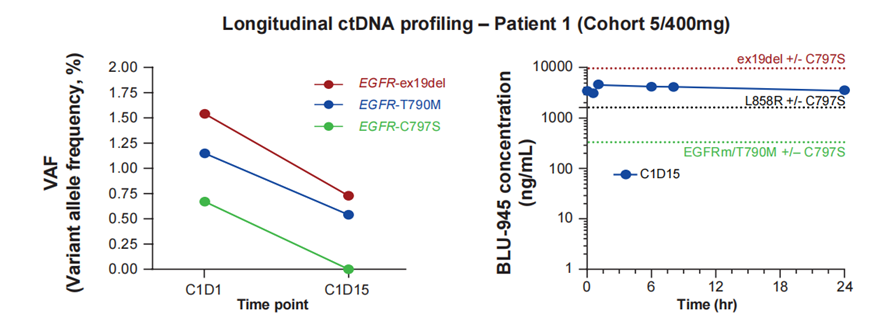
图5中的患者1,白人女性,69岁,无吸烟史,确诊时为IV期NSCLC,经历了含铂化疗,厄洛替尼和奥希替尼,最佳疗效均为疾病稳定,外周血检测结果为EGFR Del 19/T790M/C797S,多发脑,骨,肝,腹膜后和纵隔淋巴结转移。BLU-945 400mg每天一次,第15天时,三种EGFR突变含量均出现下降,其中C797S含量降至未检出,一个疗程后影像复查,肿瘤缩小30%,目前仍继续治疗中,耐受性良好。
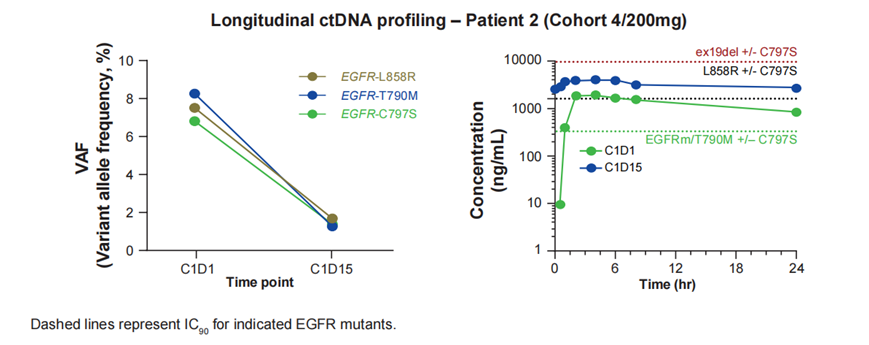
患者2,亚洲女性,70岁,无吸烟史,确诊时为IVB期NSCLC,经历了奥希替尼,赛沃替尼和含铂化疗,多发肺和左股骨转移,外周血检测结果为EGFR L858R/T790M/C797S。BLU-945 200mg每天一次,第15天时,三种EGFR突变含量均出现下降,一个疗程后影像复查,肿瘤缩小21%,二个疗程后影像复查,肿瘤继续缩小至-28%,目前仍继续治疗中。
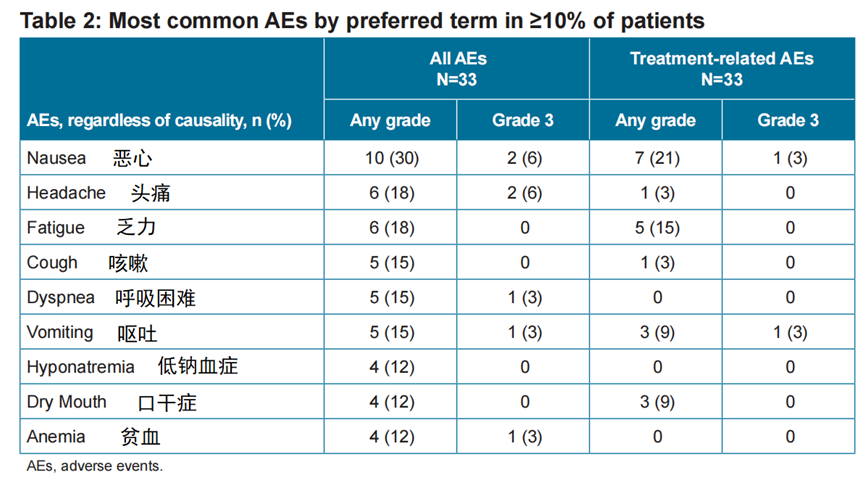
※安全性
BLU-945耐受性良好,在1期剂量爬坡试验中,没有发现4级和5级不良反应,也未发现间质性肺病和QTc间期延长事件,没有患者因不良反应而永久停药。
400mg每天一次时,发现1例剂量限制毒性,3级肝转氨酶升高,经暂停给药,症状缓解后继续服药中。
与抑制野生EGFR相关的不良反应轻微,皮疹3%,皮肤干燥3%,腹泻9%,均为1级。没有观察到甲沟炎事件。
BLU-945的最大耐受剂量仍未确定,目前正在探索600mg每天一次的剂量。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#抑制剂#
43
#结果公布#
50
#ACR#
46
#GFR#
37
#AACR#
34