Eur Heart J:冠状动脉血流储备与心血管结局
2021-11-25 MedSci原创 MedSci原创
在广泛的病理过程中,冠状动脉血流减少与全因死亡率和MACE风险增加密切相关。这一结果支持最近的建议,即在临床实践中应更常规地测量冠状动脉血流,以针对高危个体进行积极的血管风险调整。
冠状动脉血流储备(CFR)是通过运动、压力或微循环血管舒张可以增加冠状动脉血流量的比率。作为冠状动脉疾病严重程度的指标,CFR具有多种生物学和临床实践优势。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,这项荟萃分析旨在量化冠状动脉血流减少与全因死亡率和主要不良心血管事件(MACE)之间的关联,跨越了广泛的患者组别和病理机制。
研究人员全面地检索定并确定了2000年1月1日至2020年8月1日期间的所有研究,这些研究评估了冠状动脉血流并报告了患者的临床结局。该研究的终点是全因死亡率和MACE。研究人员使用随机效应模型根据公布的风险比(HR)计算效应估计值。
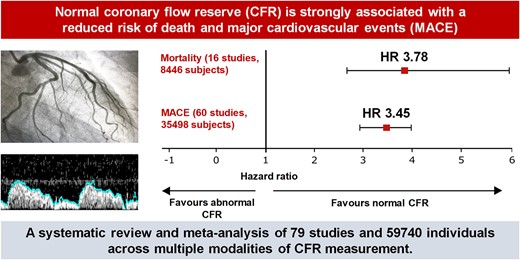
该荟萃分析共纳入了79项研究,涉及59740名受试者。冠状动脉血流储备异常(CFR)与较高的全因死亡率[HR为3.78,95%置信区间(CI)为2.39-5.97]和较高的MACE发生率(HR为3.42,95%CI为2.92-3.99)相关。CFR每降低0.1个单位与死亡率(每改变0.1个CFR单位HR为1.16,95%CI为1.04-1.29)和MACE(每改变0.1个CFR单位HR为1.08,95%CI为1.04-1.11)成比例增加相关。在孤立性冠状动脉微血管功能障碍患者中,异常CFR与较高的死亡率(HR为5.44,95%CI为3.78-7.83)和MACE发生率(HR为3.56,95%CI为2.14-5.90)相关。在急性冠脉综合征(HR为3.76,95%CI为2.35-6.00)、心力衰竭(HR为6.38,95%CI为1.95-20.90)、心脏移植(HR为3.32,95%CI为2.34-4.71)和糖尿病(HR为7.47,95%CI为3.37-16.55)患者中,异常CFR与较高的MACE发生率相关。
由此可见,在广泛的病理过程中,冠状动脉血流减少与全因死亡率和MACE风险增加密切相关。这一结果支持最近的建议,即在临床实践中应更常规地测量冠状动脉血流,以针对高危个体进行积极的血管风险调整。
原始出处:
Mihir A Kelshiker.et al.Coronary flow reserve and cardiovascular outcomes: a systematic review and meta-analysis.European Heart Journal.2021.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab775/6438087
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉血流#
38
#动脉血#
38
#心血管结局#
66
#ART#
33
#HEART#
41
自动体外除颤仪便于操作,即使非专业人员也可以安全进行除颤。
64