Appl Bionics Biomech:腰椎间盘突出症患者中医康复干预腰椎功能恢复
2022-07-15 August MedSci原创
通过增加腰神经根的牵引力,可以显着减少局部粘连,增加神经根的活动度,减轻对神经的压力。术后早期、合理、系统的康复锻炼可以刺激神经元突触,促进神经功能恢复,减少功能障碍和疼痛,降低术后腰腿痛的发生率。
腰椎间盘突出症(LDH)是一种常见的骨科疾病。是椎间盘退变、破裂、脊柱后凸压迫脊髓或神经引起的以腰腿痛为主要症状的临床综合征。腰椎间盘突出症的手术治疗效果显着,但部分患者术后会因粘连、压迫等原因复发,腰部、臀部或下肢的疼痛和肌力会再次降低。
术后及时正确的康复治疗和完善的护理,可以防止神经根粘连和受压,促进功能恢复,缩短康复时间,降低复发率。通过增加腰神经根的牵引力,可以显着减少局部粘连,增加神经根的活动度,减轻对神经的压力。术后早期、合理、系统的康复锻炼可以刺激神经元突触,促进神经功能恢复,减少功能障碍和疼痛,降低术后腰腿痛的发生率。
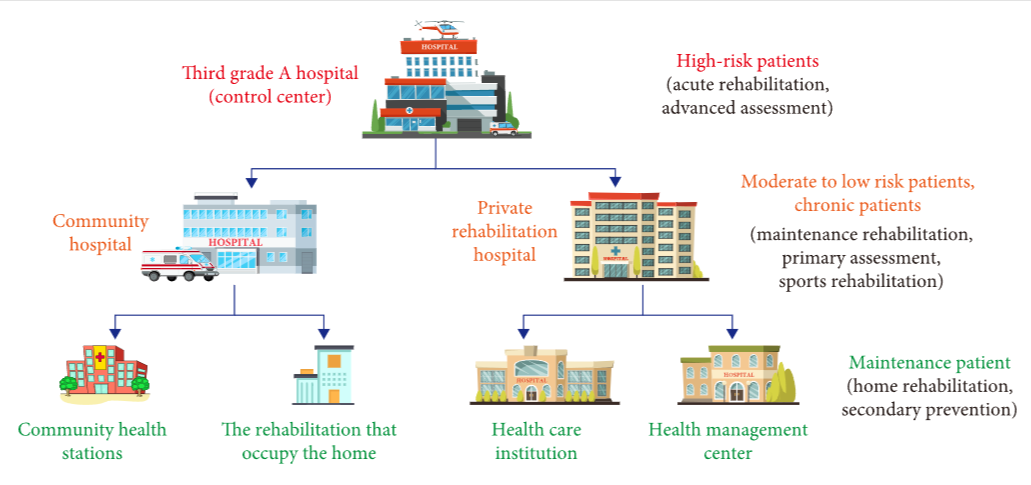
腰椎康复流程图:
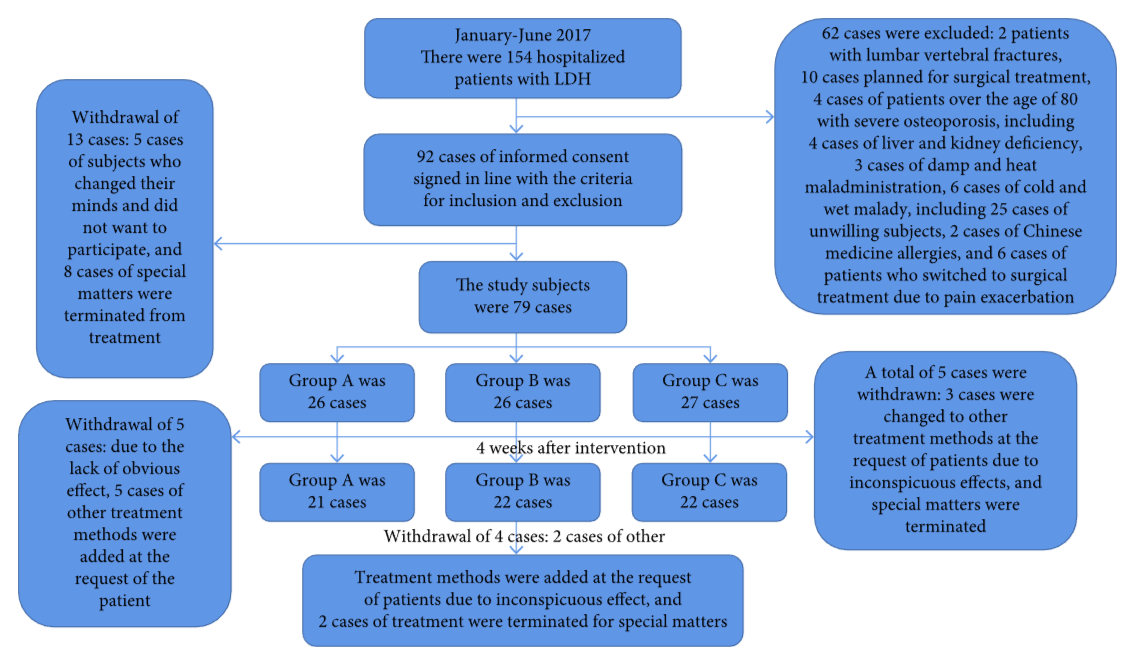
为研究中医康复治疗腰椎间盘突出症的疗效,建议将热敷、普通沙袋或热敷与中药的效果进行比较。选取某中医院气滞血瘀证符合LDH诊断标准及中医诊断疗效标准证候分类的患者79例。将受试者随机分为A、B、C组:A组(26例)为沙袋热敷干预组,接受简单沙袋热敷方案;B组(26例)为单纯中药热敷干预组,接受中药热敷方案;C组(27例)为中药沙袋联合热敷干预组,接受中药沙袋联合热敷方案。三组除了使用不同的热压介质外,其他方面保持不变。每次热敷的治疗时间为 40 分钟,每天两次,持续 2 周。干预过程中共有14例脱落,65名受试者完成干预过程。实验表明,三组之间没有显着差异(P > 0.05)。测试结果得到证实。
研究对象的选择和确定过程:
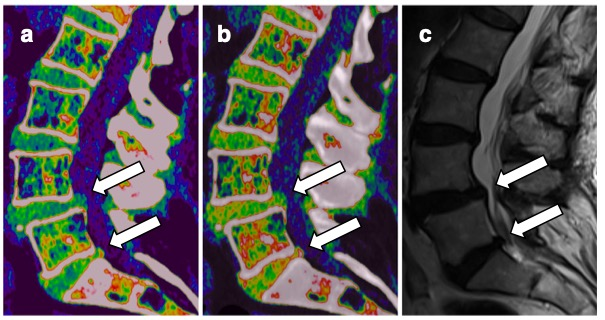
技术路线图:

研究中发现依从性总体良好,原因如下:(1)湿敷治疗不仅疗效确切,能有效缓解疼痛、麻木症状,而且增加了患者的舒适度由于其温暖的物理作用;(2)热敷手术无创、无痛,患者乐于接受;(3)热敷治疗的操作方法简单,临床上易于实施: (4)中药价格低廉,患者更容易经济承受。同时,国家大力发展和扶持中医药技术和医疗保险政策,为热敷治疗的实施提供了有力保障:(5)在热敷治疗过程中进行相关的健康指导,提高了患者对中医的了解和认识。因此,增加了患者的满意度和依从性。
综上所述,此研究中热敷法简单实用,副作用小,医疗费用低,疗效好,患者接受度高,患者容易收集,实验过程顺利,基本达到预期目的。针对当前研究中存在的问题,未来的研究需要纳入一些客观的标准生化指标,以及根据不同证型进行中医辨证论治。不同的热敷方法需要有明确的标准和临床路径。为了评估LDH的治疗效果,患者需要长期随访才能了解其远期效果。
原文:Yan L, Chenni W, Fang L, LiyueYang. Medical Data Analysis of Lumbar Disc Herniation Patients after Traditional Chinese Medicine Rehabilitation Intervention Lumbar Function Recovery. Appl Bionics Biomech. 2022 May 18;2022:1288233. doi: 10.1155/2022/1288233. PMID: 35634176; PMCID: PMC9132704.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Bio#
54
?
31
#椎间盘突出#
41
#腰椎#
47
#功能恢复#
41
#腰椎间盘#
52
学习
39