JCO:ASCO肿瘤患者静脉血栓防治推荐指南
2013-05-27 JCO dxy
在2013年5月20日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)上,美国临床肿瘤学会发布了最新版静脉血栓(VTE)防治推荐指南。该指南涉及内容包括门诊患者、住院患者和围手术期患者的预防,以及在针对肿瘤治疗过程中抗凝药物的治疗应用。 修订委员会对2007年12月至2012年期间,在MEDLINE及Cochrane联合图书馆上发表的相关文献进行了系统考察
在2013年5月20日在线出版的《临床肿瘤学杂志》(Journal of Clinical Oncology)上,美国临床肿瘤学会发布了最新版静脉血栓(VTE)防治推荐指南。该指南涉及内容包括门诊患者、住院患者和围手术期患者的预防,以及在针对肿瘤治疗过程中抗凝药物的治疗应用。
修订委员会对2007年12月至2012年期间,在MEDLINE及Cochrane联合图书馆上发表的相关文献进行了系统考察。为确定需要修订的推荐规范条目,修订委员会对相关实证进行了审核。最终共有42份文献符合筛选标准,其中包括16份系统性综述及24项随机对照临床试验。该指南部分摘要如下。
具体推荐规范
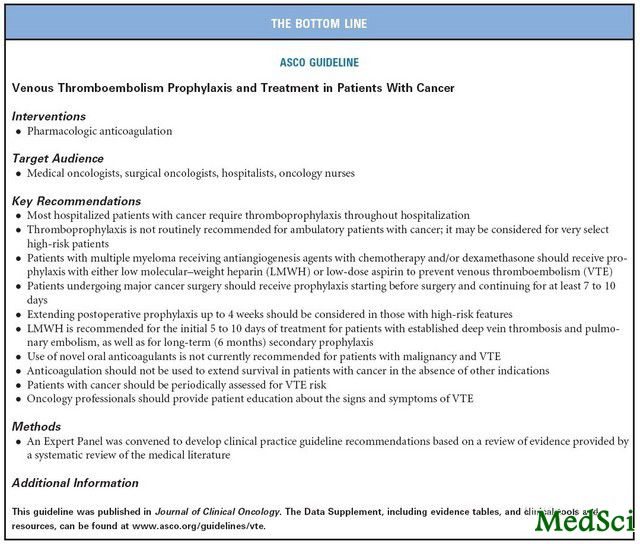
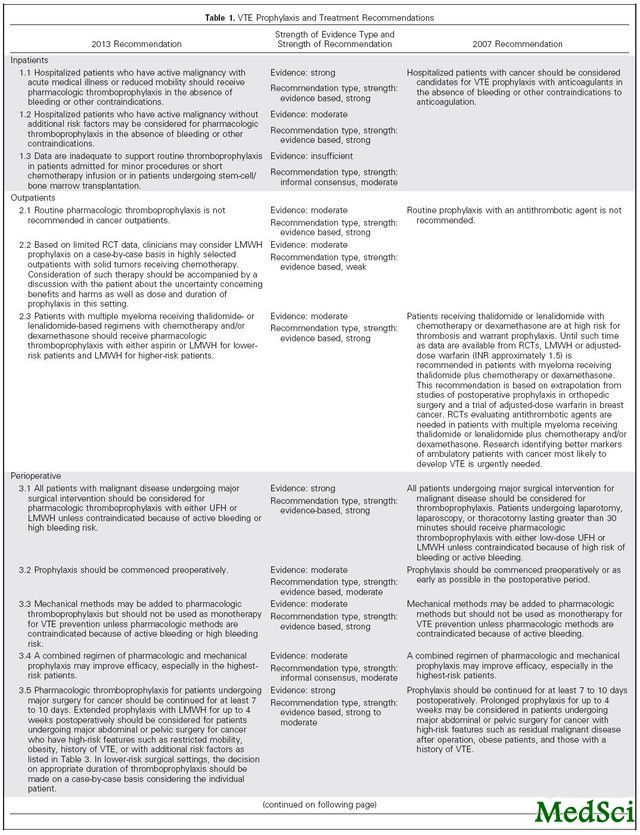
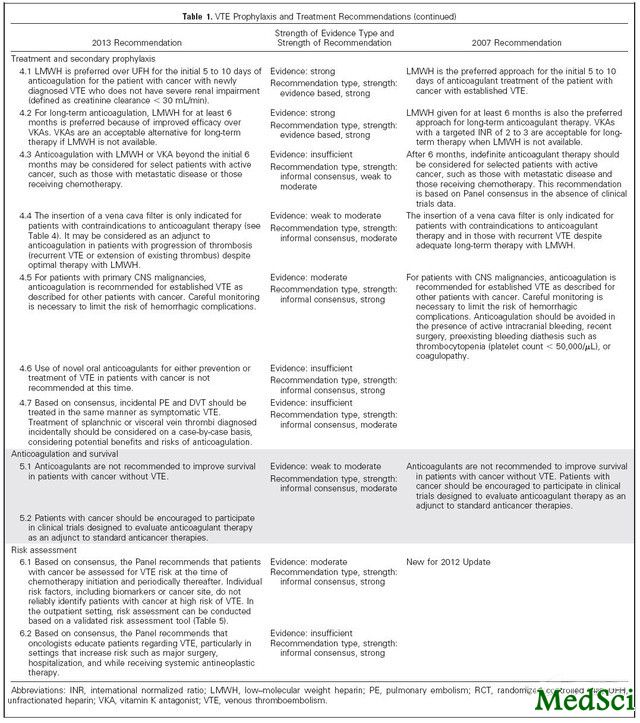
推荐规范:在住院期间,多数住院肿瘤患者需进行血栓预防。不建议门诊肿瘤患者进行日常的血栓预防。可有选择地对部分高危患者进行血栓预防。接受血管生成抑制剂联合化疗和/或地塞米松治疗的多发性骨髓瘤患者应进行血栓预防,可通过低分子量肝素或低剂量阿司匹林进行。对于接受大型肿瘤手术治疗的患者,在手术前应开始进行血栓预防,并至少持续7至10天。对于具有高危特征的患者,应考虑将预防时间延长至4周。对于深层静脉血栓、肺栓塞以及长期性(6个月)次级预防,建议使用LMWH作为最初5至10天的起始药物。目前不推荐恶性肿瘤及VTE患者使用新型口服抗凝药物。抗凝药物不应用于无其他适应症的肿瘤治疗。肿瘤患者应定期评价VTE风险。肿瘤科专业人员应就VTE征兆及症状为患者提供培训。

Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline Update.
PURPOSE
To provide recommendations about prophylaxis and treatment of venous thromboembolism (VTE) in patients with cancer. Prophylaxis in the outpatient, inpatient, and perioperative settings was considered, as were treatment and use of anticoagulation as a cancer-directed therapy.
METHODS
A systematic review of the literature published from December 2007 to December 2012 was completed in MEDLINE and the Cochrane Collaboration Library. An Update Committee reviewed evidence to determine which recommendations required revision.
Results
Forty-two publications met eligibility criteria, including 16 systematic reviews and 24 randomized controlled trials.
Recommendations
Most hospitalized patients with cancer require thromboprophylaxis throughout hospitalization. Thromboprophylaxis is not routinely recommended for outpatients with cancer. It may be considered for selected high-risk patients. Patients with multiple myeloma receiving antiangiogenesis agents with chemotherapy and/or dexamethasone should receive prophylaxis with either low-molecular weight heparin (LMWH) or low-dose aspirin. Patients undergoing major cancer surgery should receive prophylaxis, starting before surgery and continuing for at least 7 to 10 days. Extending prophylaxis up to 4 weeks should be considered in those with high-risk features. LMWH is recommended for the initial 5 to 10 days of treatment for deep vein thrombosis and pulmonary embolism as well as for long-term (6 months) secondary prophylaxis. Use of novel oral anticoagulants is not currently recommended for patients with malignancy and VTE. Anticoagulation should not be used for cancer treatment in the absence of other indications. Patients with cancer should be periodically assessed for VTE risk. Oncology professionals should provide patient education about the signs and symptoms of VTE.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
38
#静脉血#
42
#静脉#
40
#JCO#
37
#肿瘤患者#
36