JSDT:肥胖患者微创椎间孔腰椎间融合术安全可靠
2014-07-09 lining117826 丁香园
肥胖被认为是腰痛的独立危险因素。美国国立卫生研究院对肥胖的分级如下规定:BMI在25-30间为超重,30-40则为肥胖。外科医生认为,肥胖患者手术暴露困难,手术时间较非肥胖患者延长。并且,有研究认为,超重或肥胖患者行选择性脊柱融合的围手术期并发症发生率为36.9%。 目前,肥胖和非肥胖患者行微创或开放脊柱手术的研究有大量报道,然而,没有研究比较超重或肥胖患者行微创或开放椎间孔腰椎融合术的疗效
肥胖被认为是腰痛的独立危险因素。美国国立卫生研究院对肥胖的分级如下规定:BMI在25-30间为超重,30-40则为肥胖。外科医生认为,肥胖患者手术暴露困难,手术时间较非肥胖患者延长。并且,有研究认为,超重或肥胖患者行选择性脊柱融合的围手术期并发症发生率为36.9%。
目前,肥胖和非肥胖患者行微创或开放脊柱手术的研究有大量报道,然而,没有研究比较超重或肥胖患者行微创或开放椎间孔腰椎融合术的疗效差异。为了评价超重或肥胖患者行微创或开放椎间孔腰椎融合术的临床结果及安全性,来自中国三军大的学者Wang Jian等进行了一项前瞻性对比研究,该研究结果已在近期的Journal of Spinal Disorders & Techniques杂志上发表。
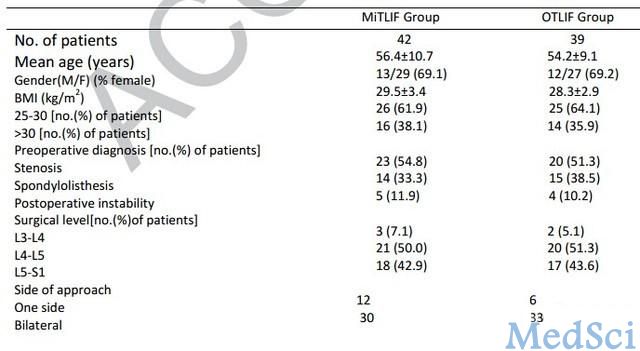
在该研究中,81例患者(25男,56女,平均年龄55.3岁)获得了随访,其中椎管狭窄患者43名,腰椎滑脱患者29名,椎板切除不稳定患者9名。患者平均随访时间为36.1月。其中,微创组42人,平均BMI为29.5,开放组39人,平均BMI为28.3(表1)

该研究表明,微创椎间孔腰椎间融合术治疗超重或肥胖患者,其疗效安全可靠。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肥胖患者#
36
#椎间孔#
35
#椎间融合术#
0
#腰椎#
33
#微创#
35
#融合#
26
#融合术#
34