Eur Radiol:造影剂所导致的GFR轻度降低是否会诱发肾损伤?
2021-03-13 shaosai MedSci原创
几十年来,对比剂引起的急性肾损伤(CI-AKI)的真实发生率和临床重要性一直存在争议。据最近的对照研究表明,CI-AKI的发生风险一直被高估。

几十年来,对比剂引起的急性肾损伤(CI-AKI)的真实发生率和临床重要性一直存在争议。据最近的对照研究表明,CI-AKI的发生风险一直被高估。在这些回顾性研究中,由于计算机断层扫描(CT)指征的差异和对照组选择偏倚,对比剂(CM)对肾功能的真实影响很难客观评价。此外,CM注射后发生的AKI可能是由与血管内CM相关的其他暂时性改变引起的。因此,无论CM是否是造成AKI的直接原因,临床上都将此类AKI称为对比剂用药后AKI (PC-AKI)。
CI-AKI的不同定义、血清肌酐(Scr)测量误差和Scr水平的个体内差异增加了研究CM对肾功能影响的难度。最近,欧洲泌尿生殖放射学会(ESUR)对比剂剂安全委员会修正了AKI的Scr标准,采用KDIGO作为最新评价标准。
近日,发表在European Radiology杂志的一项研究前瞻性的比较了注射对比剂后血清肌酐(Scr)的变化与正常个体内Scr波动确定了随机选择的大样本人群中PC-AKI的发生率,以更科学的方法解释了CM对肾功能影响并更客观的评价了PC-AKI的真实发生率。
在本项前瞻性研究中,共纳入了瑞典CArdio肺生物图像研究(SCAPIS)机构的1009名参与者(年龄在50-65岁之间,女性占48%),预计肾小球滤过率(eGFR)≥50 mL / min,所有受试者均在冠状动脉CT血管造影(CCTA)时接受标准剂量的静脉注射碘海醇。在CCTA前取得了两个独立Scr样本,以及CCTA后2-4天的一个随访样本。对Scr的变化进行统计学分析,并对可能的危险因素进行分层。
行CCTA后Scr的中位数增加0-2μmol/ L。根据旧的ESUR标准(Scr增加> 25%或> 44μmol/ L )在1009个人中观察到12个人表现出PC-AKI(1.2%),而在使用更新的ESUR标准时在1009个人中观察到2个人(0.2%)表现出PC-AKI (Scr增加≥50%或≥27μmol/ L)。可能的危险因素(例如糖尿病、年龄、eGFR、使用NSAID)并未显示出发生PC-AKI的风险增加。对比剂对Scr的平均影响不超过个体的Scr波动。
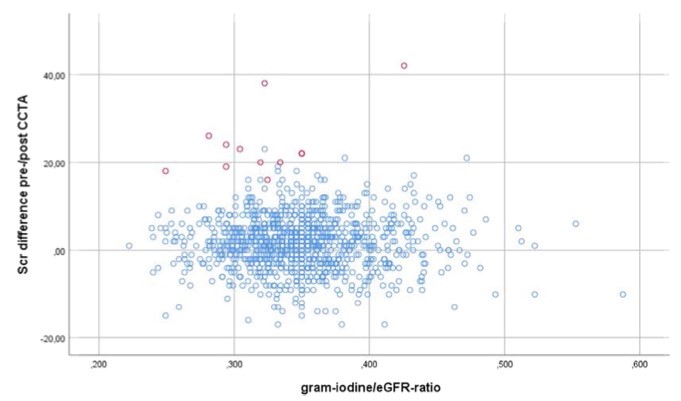
图 CCTA前后血清肌酐(Scr)的差异与碘海醇/ eGFR(估计肾小球滤过率)的比值的关系。对比剂用药后发生急性肾损伤(PC-AKI)病例( Scr增高> 25%)显示为红色。
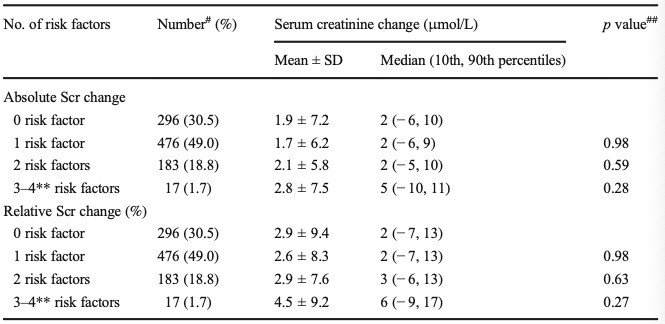
表 与第二次行CCTA前Scr值相比,行CCTA后(冠状动脉CT血管造影)血清肌酐(Scr)的变化,并按危险因素数量进行了分层。
发生PC-AKI的风险很低(1.2%),当使用最新的ESUR标准时甚至更低(0.2%)。本研究表明eGFR≥45 mL/min/1.73 m2的患者发生PC-AKI的风险较小。与没有危险因素的人相比,有潜在危险因素如糖尿病或非甾体抗炎药使用史的人,并没有显示出更明显的Scr增加。CM对Scr的平均影响不超过个体内Scr的波动。对于目前CM剂量和碘海醇剂量/eGFR比值低于0.6的轻度肾功能下降的患者,静脉注射碘海醇行相应检查是相对安全的。与旧的标准相比,应用ESUR更新的PC-AKI标准所诊断PC-AKI病例更少。
原始出处:
Jeanette Carlqvist,Ulf Nyman,Gunnar Sterner,et al. Minimal risk of contrast-induced kidney injury in a randomly selected cohort with mildly reduced GFR.PMID:33155105DOI:10.1007/s00330-020-07429-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#损伤#
25
#造影#
36
#GFR#
0
多谢分享
68