Semin Arthritis Rheu:湖北省IgG4-RD患者COVID-19 感染的临床特征
2020-05-20 xiangting MedSci原创
IgG4-RD患者属于COVID-19感染的易感人群,因此需要更细致的个人防护。
IgG4相关性疾病(IgG4-RD)是一种免疫介导的多器官、慢性进行性疾病。这项研究旨在调查湖北省IgG4-RD患者中COVID-19的易感性,并描述IgG4-RD患者COVID-19的临床表现。
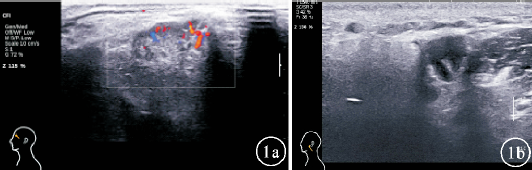
一个随访系统纳入了过去10年间全国200多例IgG4-RD患者。共有91例生活在中国湖北的IgG4-RD患者对此项调查做出了回应。通过标准化的数据收集表格获得病史、临床症状、实验室检查、CT影像和治疗,然后由两名研究者独立进行审核。
91例患者中有2例感染了COVID-19。这两人均被归类为中等类型。诸如发烧、咳嗽的症状和影像学特征与其他COVID-19患者相似。这2例患者在连续口服小剂量糖皮质激素的情况下,均未出现IgG4-RD复发,也没有发展为严重或重症COVID-19。另外,2号患者SARS-CoV-2核酸转阴的时间很长。
IgG4-RD患者属于COVID-19感染的易感人群,因此需要更细致的个人防护。早期识别和适当治疗对于防止感染COVID-19的IgG4-RD患者发展为重症非常重要。
原始出处:
Yu Chen. Clinical characteristics of IgG4-RD patients infected with COVID-19 in Hubei, China. Semin Arthritis Rheu. 16 May 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#临床特征#
30
#Arthritis#
32
#ART#
27
#IgG4#
24
#IgG#
26
希望患者能撑过去
81