CORR:内固定和半髋治疗股骨颈骨折长期疗效无差异
2014-02-18 小小老虎 dxy
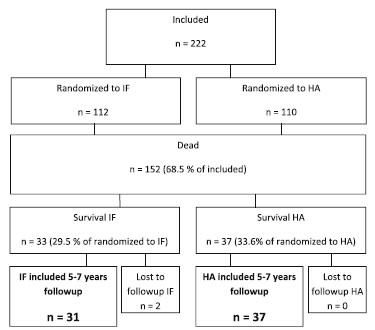
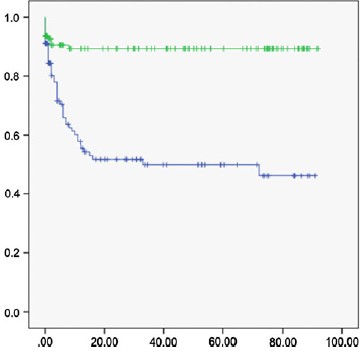
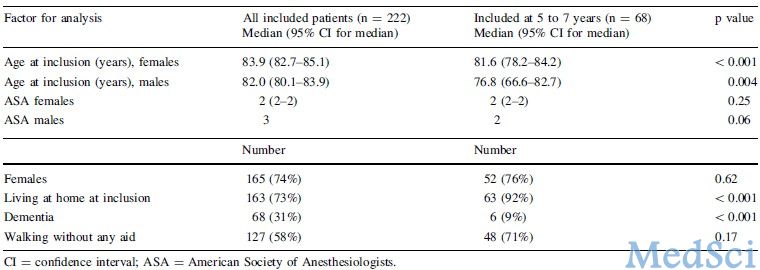
在所有骨科损伤中,髋部骨折的致残率和死亡率高居榜首,与其相关的医疗费用也非常惊人。有人预测随着老龄化的发展,到2025年,全球老年髋部骨折患者人数将接近4百万。按照骨折位置进行分类,髋部骨折可分为关节囊内的股骨颈骨折和关节囊外的转子间和转子下骨折,其中一半的髋部骨折是股骨颈骨折。【原文下载】 从20世纪初开始,对于囊内股骨颈骨折的治疗方法一直存在争议。内固定治疗可保留患者骨质,手术简

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#股骨颈#
43
#股骨#
36
#内固定#
41
#长期疗效#
36
#股骨颈骨折#
34
#ORR#
34