患者资料
患者老年女性、74岁、回族,搀扶老伴起床时突感胸背部疼痛5天后入院。既往患有糖尿病、颈椎病、腰椎管狭窄症、多发性脑梗塞等慢性疾病史;50岁绝经。
入院查体:一般情况良好,心肺腹无异常,专科查体胸腰段轻度后凸畸形,T10-12椎体棘突压痛明显,无双下肢神经症状,患者主要为翻身疼痛明显,站立行走疼痛可忍受,影响日常生活。
入院后完善各项检查。
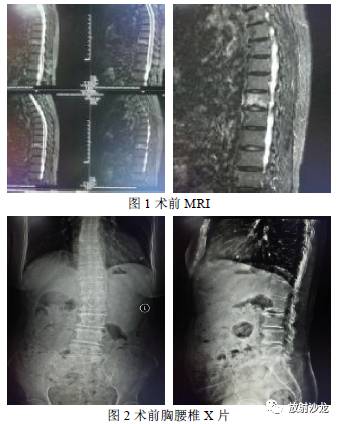
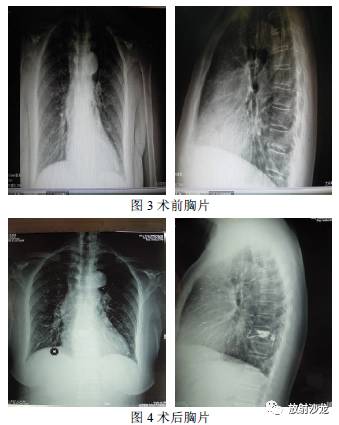
行胸腰椎MRI检查(图1)明确诊断为T10椎体骨折、骨髓水肿;入院后第5天在局麻下行T10椎体成形术,术中定位、穿刺等操作顺利,手术历时30分钟,手术过程中患者除穿刺时有疼痛主诉外无任何不适反应,注入骨水泥过程中发现椎体前缘血管渗漏立即终止手术,询问患者无不适,待水泥凝固后拔出工作套管,C臂透视显示椎体前缘有血管影,椎体后方无渗漏,送患者回病房,心电监护、密切监测生命体征24小时,患者无不适,术后疼痛立刻缓解,可自由翻身,术后第1日带腰围下地行走,常规使用抗骨质疏松治疗3天出院(静脉滴注唑来膦酸钠5mg:100mL)。
出院前复查术后X光片(图4)发现双肺多发散在毛细血管显影,考虑为骨水泥渗漏、肺栓塞,出院后跟踪电话随访患者无肺部症状,考虑为无症状性骨水泥肺栓塞。继续追踪随访。本例患者虽未造成严重不良后果,但我们应该高度重视此并发症,一旦发生严重事件,后果不堪设想,故撰写此文以提醒同行,以免发生不可挽回的损失。
 讨论
讨论
经皮后路椎体成形术治疗老年性OVCFs为目前治疗骨质疏松性椎体骨折的主要手段之一,因其在改善患者病椎周围症状、提高生存质量以及镇痛等方面比保守治疗方法有较明显的疗效而被临床广泛应用,由此带来的并发症也随之越来越被学者关注,本例患者为非常典型的骨水泥在注入过程中渗漏入椎旁血管,并通过腔静脉系统回流至右心室进而进入肺动脉造成肺栓塞。有报道称该手术所发生的重度并发症包括:骨水泥渗漏至椎旁静脉引起的肺栓塞、心脏穿孔、脑栓塞、甚至死亡等病例。
笔者通过亲历临床病例并查阅大量文献后认为PVP、PKP目前作为治疗骨质疏松性椎体骨折的疗效已通过大量的临床验证,其微创、有效等特点毋庸置疑,但对该手术造成的并发症仍然需慎重考虑,为避免严重并发症发生,通过文献资料本人对此做一简单概括:术前检查需慎重,不可轻视该手术为小手术而关注度不高,凝血功能、心肺等检查需评估;
必要时行CT检查了解椎体前后缘有无破损等,为手术操作及注入骨水泥时机提供临床资料,术者做到心中有数,而不至于盲目手术操作造成并发症发生;手术操作要熟练,避免反复穿刺,给骨水泥渗漏提供通道,尤其在穿刺过程中不慎误进椎管而为骨水泥渗漏至椎管内创造条件,如穿刺发现有脑脊液流出,立即改变穿刺方向,注入骨水泥时应避免渗漏至椎管;助手及跟台护士须有良好的专业知识及配合经验,关键步骤术者亲自把关,不可轻信厂商跟台人员或器械护士,尤其是“新人”更应提高警惕;注入骨水泥时动作轻柔,不可压力过大,注射应在拉丝期或拉丝后期比较合适,及时透视监视骨水泥注入情况,如有渗漏,根据情况缓慢注入或停止手术,如发现椎体血管渗漏,立即终止手术,密切观察患者生命体征,做好抢救准备工作;术中频繁与患者沟通,如患者有呼吸困难、心慌、胸闷、胸前区疼痛、血压下降等异常表现,随时终止手术,进一步观察;在监护下完成手术、建立静脉通道。
笔者认为只要遵循上述几点注意事项并严格执行,大部分并发症是可以避免发生的,除非患者特异体质,对骨水泥过敏等难以避免外。虽然椎体成形术造成骨水泥渗漏并不少见,大多未造成严重后果,为了避免骨水泥性肺栓塞等严重并发症的发生,还需引起临床医生的高度重视。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#并发#
33
#椎体骨折#
47
#椎体#
40
#无症状#
26
#骨质#
29