J Ebdovasc Ther:CH-EVAR治疗无症状dPAA患者的多中心研究结果
2021-11-15 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
近年来,烟囱技术腔内腹主动脉瘤修复术(CH-EVAR)在复杂AAA和其他肾旁主动脉瘤(dPAA)病变的治疗中的作用迅速发展。CH-EVAR随之备受重视,并且被纳入到了最新SVS和ESVS指南。值得注意
近年来,烟囱技术腔内腹主动脉瘤修复术(CH-EVAR)在复杂AAA和其他肾旁主动脉瘤(dPAA)病变的治疗中的作用迅速发展。CH-EVAR随之备受重视,并且被纳入到了最新SVS和ESVS指南。值得注意的是,CH-EVAR主要被证明是紧急情况下的替代方案,并且理想情况下烟囱支架应不超过2枚,其早无症状dPAA患者群体中的治疗作用尚不明确。Pitoulias等评估了择期CH-EVAR治疗无症状dPAA患者的疗效,结果发表于J Endovasc Ther。
研究目的
评估择期CH-EVAR治疗无症状dPAA患者的疗效。
研究方法
2008~2014年,对在13个欧美国家的医学中心接受择期CH-EVAR手术治疗的患者进行分析。共517例患者接受CH-EVAR手术,其中326例dPAA患者;排除有症状和/或破裂患者后,剩余275例无症状dPAA患者;另有8例患者失访,最终纳入267例dPAA患者纳入本次回顾性分析。主要终点是30天和出院CH-EVAR相关死亡率。次要终点包括持续性Ia型内漏、造影证实的闭塞和/或烟囱移植物(CG)或累及内脏血管狭窄,以及CH-EVAR相关再干预。
研究结果
267例患者的平均年龄为75.2±7.4岁,男性比例为82.0%,供累及内脏血管442条。术中6条肾动脉被主动脉移植物有计划的覆盖,其余436条血管均被重建。即刻技术成功率为98.6%。
主要终点结果:术后30天死亡率为1.9%(n=5),院内并发症发生率为10.1%(n=27),包括3例中风、1例永久性透析和1例肠缺血。30 天内为检测到 Ia 型内漏。总体死亡率为21.0%(n=56)(表1)。Kaplan-Meier生存曲线评估3年总体生存率为75.0±0.2%,免于CH-EVAR相关死亡率为98.0±0.1%(图1)。

表1. 并发症和死亡的详情

图1. Kaplan-Meier生存曲线
次要终点结果:术中7条内脏血管闭塞,其中仅1条为CH-EVAR相关的CG闭塞。30天内,有6例患者的7枚CG发生阻塞(表2)。平均随访25.5±13.3个月,期间AAA最大直径显着减小。随访期间,总体原发性和继发性 Ia 型内漏发生率分别为8.2% 和 5.6%。CG一期通畅率为87.0%,二期通畅率为89.0%(图2)。
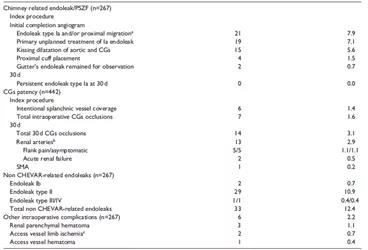
表2. 术后30天内主要结果
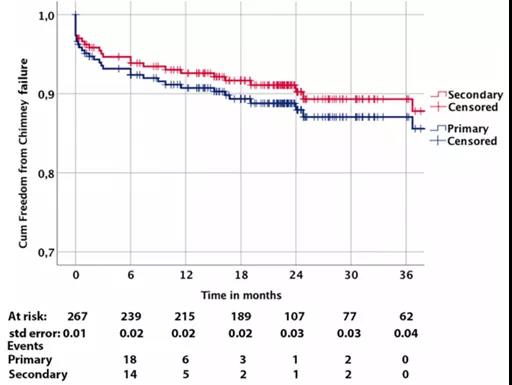
图2. 一期和二期通畅率的Kaplan-Meier曲线
总 结
针对dPAA的治疗,择期CH-EVAR手术持久有效。本研究结果与其他已发表的腔内治疗结果相当,这也证明了CH-EVAR在治疗无症状dPAA患者中有一定的应用前景。
原始出处:
Pitoulias G, Fazzini S, Donas K, et al. Multicenter Mid-Term Outcomes of the Chimney Technique in the Elective Treatment of Degenerative Pararenal Aortic Aneurysms. J Ebdovasc Ther. 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#多中心#
30
#研究结果#
25
#ASC#
28
#多中心研究#
41
#无症状#
28