JACC:肾功能轻度受损对接受多血管冠状动脉血运重建手术的患者预后没有影响
2022-04-06 网络 网络
在通过PCI或CABG进行血管重建的多血管疾病患者中,肾功能轻度下降与主要综合结果和死亡率的风险增加没有明显关系。
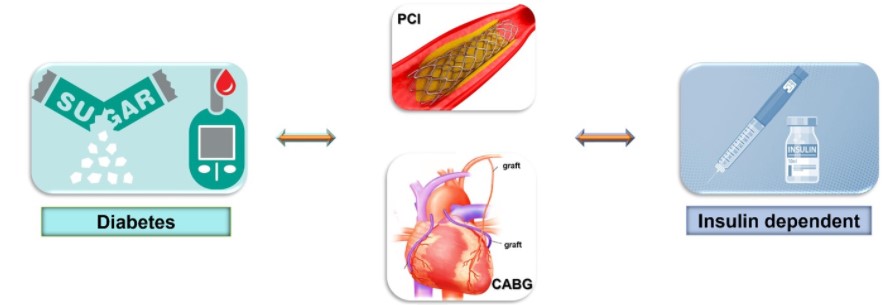
冠状动脉复杂病变的血运重建治疗常会面临治疗策略选择的困境。时至今日,经皮冠状动脉介入术(PCI)几乎可以处理所有的冠状动脉病变,但对于多支弥散病变、左主干病变以及解剖结构不适合PCI治疗则存在手术时间长、风险高、成功率低、远期效果欠佳等多重问题。
传统的冠状动脉旁路移植术(CABG)治疗不受病变血管条件的影响,且有较好的整体远期效果,但仍存在创伤大、大隐静脉桥寿命欠佳等缺点,合并多重器官疾病的老年患者难耐受手术。
截至目前,接受冠状动脉血运重建手术的患者,其肾功能轻度下降的长期预后影响仍是未知的。为了调查肾功能轻度下降的长期预后影响,以及在这样的风险群体中进行经PCI或CABG后的比较结果,来自韩国的学者开展了相关研究,结果发表在JACC杂志上。
从牙山医疗中心-多血管再通手术登记处,10354名符合条件的接受冠状动脉再通手术的患者根据估计的肾小球滤过率被分为3组(I期[n = 3735]:肾功能正常;II期[n = 5122]:轻度功能障碍;III期[n = 1497]:中度功能障碍)。主要结果是死亡、自发性心肌梗死或中风的复合结果。倾向性评分匹配被用来组建具有相似基线特征的患者队列。
结果显示,倾向性匹配后,I期和II期组的主要综合结果的风险没有差异(HR:1.12;95%CI:0.97-1.30)。然而,III期组的主要结果风险明显高于I期组(HR:1.50;95%CI:1.22-1.84)。在I、II、III期各肾功能组的匹配队列中,PCI与CABG对主要结局的相对影响相似。
II期与I期肾功能不全患者结局没有差异
综上,在通过PCI或CABG进行血管重建的多血管疾病患者中,肾功能轻度下降与主要综合结果和死亡率的风险增加没有明显关系。在边缘风险组中,PCI和CABG术后的比较结果是相似的。
参考文献:
Prognostic Impact of Mildly Impaired Renal Function in Patients Undergoing Multivessel Coronary Revascularization. J Am Coll Cardiol. 2022 Apr, 79 (13) 1270–1284
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#轻度受损#
43
#肾功能#
51
#患者预后#
40
#JACC#
37
#动脉血#
43
谢谢分享
57
#ACC#
31