

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




淋巴瘤是淋巴造血系统的一种常见肿瘤,往往可以发生在人体除了头发和指甲以外的任何器官。那生了淋巴瘤应该怎么治疗呢?这个问题还真不容易回答。总体来说,淋巴瘤的治疗应该是以化疗为主的综合治疗,但具体到某一个特定患者的治疗的时候,到底应该采用哪种具体方法或者哪些药物,其决定性因素是这个肿瘤的具体病理类型。因为淋巴瘤是原发淋巴系统的一类恶性肿瘤的总称,它不是一个单独的疾病,还包括非常多的亚型。根据2016年
本研究旨在验证18F-FDG PET 标记物可用来早期发现肝脏肿瘤小鼠模型肝肿瘤不可逆性电穿孔(IRE)的治疗反应,并将结果发表在Radiology上。
肿瘤本身及其治疗均可出现紧急情况,迅速有效处理各类肿瘤急症,避免发生死亡或严重的永久性损害是肿瘤科医生的一项高难度的挑战。现总结常见急症并发症处理要点,以供参考。动态针分割线一、上腔静脉综合征上腔静脉综合征是通往右心房的上腔静脉血流受阻引发的一系列症状,为临床最常见的肿瘤急症。主要症状:呼吸困难、面部肿胀、咳嗽、头痛、视物不清、声嘶、鼻塞、舌头肿大、恶心、头晕和喘鸣;主要体征:颈静脉怒张、上肢水
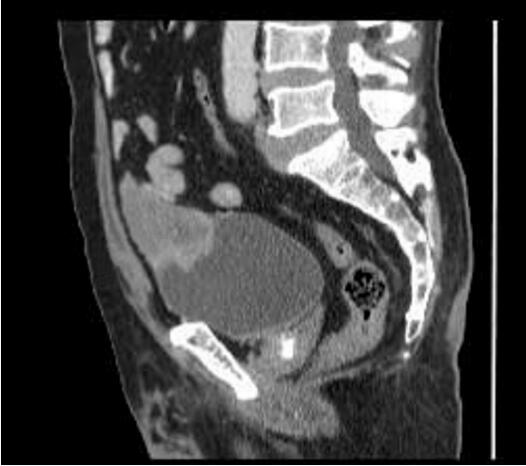
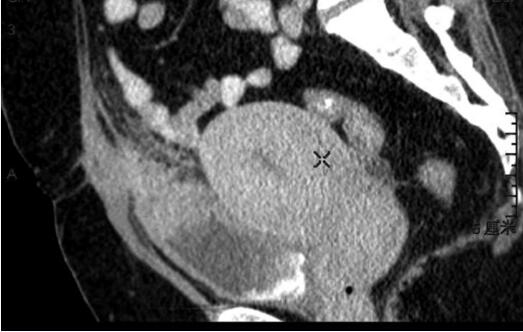
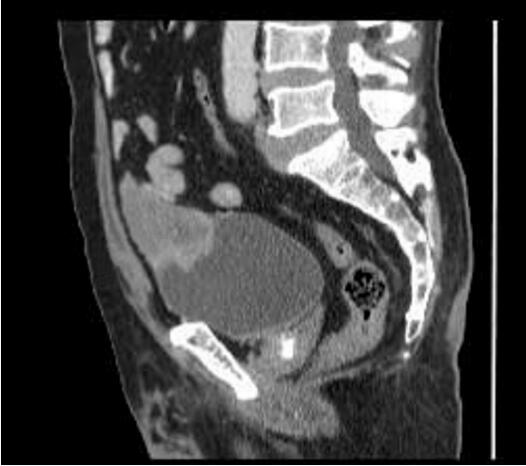
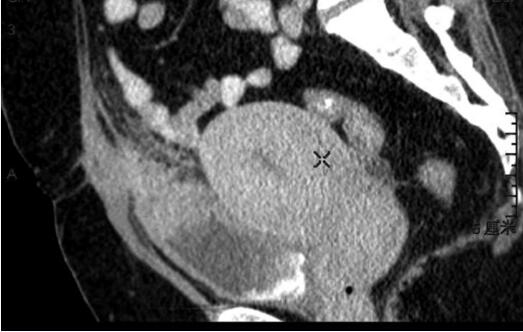
问:对于只有一个肾脏的患者,如果单肾长肿瘤,可以手术吗?答:日前,仁济医院刘东明团队成功为一名72岁独肾肿瘤患者施行了零缺血保肾手术。不阻断肾脏血流进行肾脏肿瘤切除,是保护肾脏功能的有效手段。日前,仁济医院刘东明团队运用3D影像定位靶点血管,成功为一名72岁独肾肿瘤患者施行了零缺血保肾手术。患者仅剩的一个肾脏上的四个肿瘤被安全切除,其中最大35毫米,帮助患者改变了因肾脏切除而须永久依赖透析存活的
这项大规模队列研究证实,维生素D浓度升高可降低肿瘤风险,本研究结果支持维生素D对肿瘤的预防效果
科学家们已经研制出一种可注射的凝胶状支架,同时可以结合化疗免疫治疗药物,并按顺序将它们送到局部的肿瘤中。到目前为止,动物模型的结果表明,这种方法有一天可以提高肿瘤患者或切除原发肿瘤患者的治疗效果。


梅斯医学MedSci APP
医路相伴,成就大医
#膀胱肿瘤#
47
#肿物#
42
#罕见#
39
学习
68
不错.谢谢分享
70
学习了谢
79