Front Neurosci:在年龄相关的听力损失中,维他命A、C、E和Mg++组合口服能够改善听觉阈值
2018-08-21 AlexYang MedSci原创
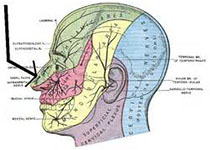
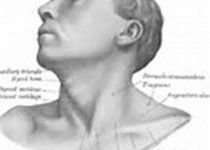
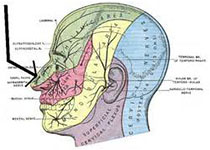
目前,年龄相关的听力损失(ARHL)增长速度加快,且伴随随后生活质量的下降和健康治疗的花费的增加,因此,需要新的治疗策略来减少和延迟该疾病造成的影响。最近,有研究人员调查了是否ARHL可以通过抗氧化物维他命A、C和E的自由基清除作用,加以Mg++组合使用(一个已知的有效的耳蜗血管舒张药(ACEMg)),能够减少ARHL产生的影响。研究包括了2个小组,ND组(正常饮食组)和ED组(包含上述药物组),
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#年龄相关#
24
#听力#
29
#ROS#
40
#阈值#
0
韩文刚,学习了!
56
学习了
41
学习了
61
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
49
学习了
40