内分泌协会年会:BPS增加乳腺癌风险
2017-04-02 MedSci MedSci原创
一项新的研究发现,双酚S(BPS)是塑料行业中化学双酚A(BPA)的替代品,显示了通过其作为内分泌干扰化学品的行为来增加乳腺癌的侵袭性的潜力。
Katie Aleck在2017年佛罗里达州奥兰多举行的第99届内分泌协会年会上向我们介绍了BPS在人类乳腺癌细胞中的新发现。BPS(双酚S)是塑料行业中化工原料双酚A(BPA)的替代品,研究发现,BPS通过干扰内分泌增加乳腺癌的侵袭性。
人们最早从聚碳酸酯硬塑料中发现了BPS,这是一种已知的内分泌干扰物质,怀疑有多种可能的健康风险。货币单据和热敏纸收据以及许多产品都宣称不含BPA。
该项研究的首席研究员,罗彻斯特奥克兰大学健康科学学院副教授Sumi Dinda博士说:"尽管希望BPS是一种更加安全的替代品,但研究显示BPS表现出的雌激素模拟行为与BPA类似。"
他们的研究证实,BPS在乳腺癌细胞中表现为雌激素样作用,Dinda补充道:"到目前为止,BPS似乎是一种有效的内分泌干扰物。"
他和他的同事研究了BPS对雌激素受体α和BRCA1基因的影响。根据国家癌症研究所的报告显示,大多数乳腺癌是雌激素受体阳性, 55%至65%的BRCA1基因有害突变的妇女会发展成乳腺癌。
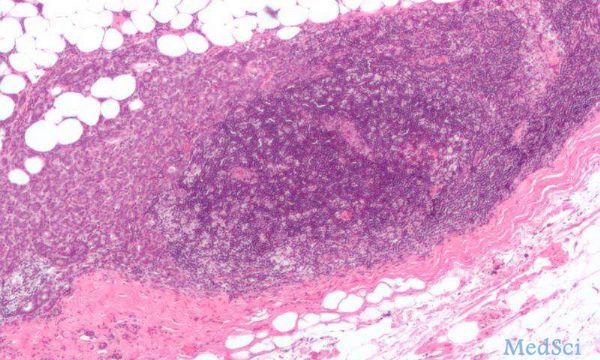
研究团队利用两种获得的商业上可获得的乳腺癌细胞系,来源为雌激素受体阳性乳腺癌妇女体内,将癌细胞暴露于不同强度的BPS或非活性物质中,其中非活性物质组为对照组。
研究人员还用雌二醇(雌激素)治疗乳腺癌细胞,发现BPS在增殖乳腺癌细胞方面起着雌激素样作用,Dinda说。 与对照相比,BPS与雌激素一样,在24小时后提高了雌激素受体和BRCA1的蛋白表达。在BPS治疗6天后,两种细胞系中的乳腺癌细胞数量在最低剂量(4微摩尔)下增加了12%,在8微摩尔下增加了60%。
研究小组然后通过用抗雌激素药物处理细胞来阻断乳腺癌细胞的BPS诱导的增殖,用于阻断雌激素对乳腺癌细胞中雌激素结合蛋白(雌激素受体)的作用。
Dinda说他们的研究结果表明BPS可能导致乳腺癌变得更具侵袭性。虽然需要对乳腺癌细胞中BPS进行进一步研究确认,但他认为"如果一名女性患有BRAC1基因突变并使用含有BPS的产品,那么发展乳腺癌的风险可能会进一步增加。"
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#癌风险#
33
#BPS#
32
#乳腺癌风险#
32
#分泌#
37