Cell Stem Cell:日本研制新方法可大量廉价制作血小板
2014-02-15 佚名 爱医
京都大学的研究小组在14日的美国《细胞-干细胞》CellStemCell 杂志网络版上报告称,他们利用能够发育成各种组织和脏器细胞的iPS细胞,成功开发出了在短时间内大量廉价制作血小板的方法。这一成果将有利于稳定供应输血时所需的血小板。 日本研制新方法可大量廉价制作血小板血小板是血液细胞之一,能够凝固血液,防止出血,手术时使用的血小板现在完全依赖献血,但是通过献血获得的血小板在室温下只能保存约4天
京都大学的研究小组在14日的美国《细胞-干细胞》CellStemCell 杂志网络版上报告称,他们利用能够发育成各种组织和脏器细胞的iPS细胞,成功开发出了在短时间内大量廉价制作血小板的方法。这一成果将有利于稳定供应输血时所需的血小板。
日本研制新方法可大量廉价制作血小板
血小板是血液细胞之一,能够凝固血液,防止出血,手术时使用的血小板现在完全依赖献血,但是通过献血获得的血小板在室温下只能保存约4天。
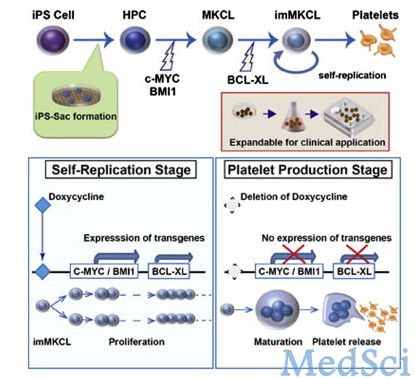
尽管此前其他研究队伍也利用iPS细胞制作出了血小板,但是由于培育出的巨核细胞的增殖能力有限,所以难以用较低的成本大量获得血小板。京都大学iPS细胞研究所教授江藤浩之率领的研究小组,利用iPS细胞培养出造血前体细胞之后,向其植入c-MYC和BMI1这两种基因,两周时间后,再追加植入BCL-XL基因,结果成功地制作出了几乎可以无限增殖的巨核细胞。让这三种基因停止发挥作用后,巨核细胞就开始制作血小板。由于能够稳定增加巨核细胞,制作血小板的效率相当于以前技术的100倍以上,制造成本也大幅降低。
由于巨核细胞非常稳定,几乎可以无限增殖,因此能够大量生产血小板,单次输血时所需的1000亿个血小板5天时间就可以准备好。这种巨核细胞在被冷冻保存数月时间后,依然能够制造血小板。虽然与从人体内采集的血小板相比止血功能尚差一些,不过研究小组认为,通过增加用量,能够弥补性能上的差距。
研究小组准备以血小板减少症为对象,在2年后开始临床研究,争取在10年后达到实用化。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#stem cell#
31
#新方法#
24
#CEL#
33
#Cell#
25
#日本#
25
#STEM#
26
小日本真强得很,尤其干细胞领域,确实处于依靠位置
144