CCQO:院外心脏停搏患者生存结局得到显著改善,但仍存在区域差异
2015-01-30 MedSci MedSci原创
莫纳什大学Nehme Z等人通过对维多利亚急救心脏停搏注册表的数据研究,地域和时间跨度上分析了心肺复苏的趋势,事件生存率,出院生存率,研究成果发表在1月份Circulation Cardiovascular quality and outcomes期刊上。 背景:虽然临床登记的价值已经在发达国家得到了很好的认可,但是其用于衡量急诊医疗质量仍然比较陌生。研究提出了一个全州急诊医疗监督举
莫纳什大学Nehme Z等人通过对维多利亚急救心脏停搏注册表的数据研究,地域和时间跨度上分析了心肺复苏的趋势,事件生存率,出院生存率,研究成果发表在1月份Circulation Cardiovascular quality and outcomes期刊上。
背景:虽然临床登记的价值已经在发达国家得到了很好的认可,但是其用于衡量急诊医疗质量仍然比较陌生。研究提出了一个全州急诊医疗监督举措,用来衡量院外心脏停搏患者的医疗护理系统质量。
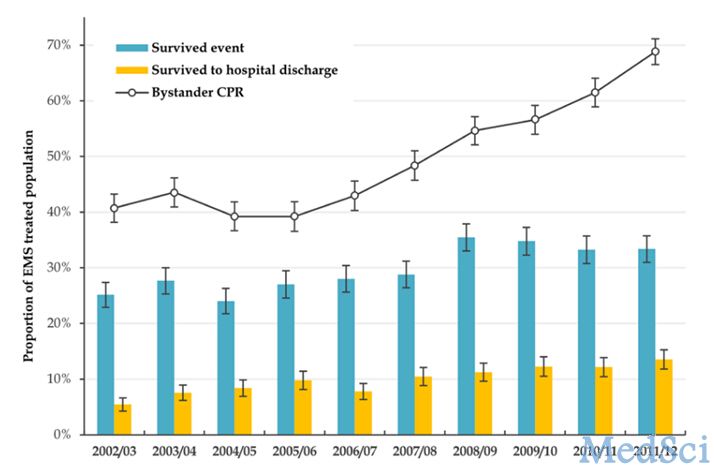
方法和结果:2002年1月1日至2012年1月30日期间,在澳大利亚东南部维多利亚州,从维多利亚急救心脏停搏注册表中,选取心源性院外心脏停搏的患者数据。从区域和时间跨度上对旁观者心肺复苏生存率,以及出院存活率进行logistic回归分析和多水平模型分析。收录32097例院外心脏停搏患者,其中14083例(占43.9%)接受了急诊医疗服务。旁观者心肺复苏后的风险调整比率(OR=2.96;95%可信区间为2.62-3.33),生存率(OR=1.55;95%可信区间1.30-1.85),出院生存率(OR=2.81;95%可信区间2.07-3.82)2011年至2012年相对于基线水平显著升高。跨区域观测旁观者心肺复苏显著变化和生存率可知,乡村地区心脏停搏患者不太可能存活至出院。存活至出院的院内变化平均OR值为1.70。
结局:2002年至2012年期间,澳大利亚维多利亚州,旁观者心肺复苏院外心脏停搏患者生存结局得到显著改善。但是,区域生存差异和院内变化在未来对患者的护理中仍然是一项重大的挑战。
原始出处:
Nehme Z, Bernard S, Cameron P, Bray JE, Meredith IT, Lijovic M, Smith K. Using a cardiac arrest registry to measure the quality of emergency medical service care: decade of findings from the victorian ambulance cardiac arrest registry. Circulation Cardiovascular quality and outcomes. 2015, Jan;8(1):56-66.
本文是MedSci原创,欢迎转载,转载请注明出处,非常感谢!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心脏停搏#
33
#患者生存#
39
提高了不少
96
已阅
55
明白
161
整体水平提升
105