NEJM:晚期黑色素瘤会抵抗PD-1 阻断治疗
2016-07-22 佚名 生物谷
近日,加州大学洛杉矶分校研究人员发现一种机制,该机制确定了晚期黑色素瘤是如何对免疫检查点抑制剂进行抵抗的,这一发现可能会引起设计新型治疗方案来治疗致命的皮肤癌。“免疫疗法可让我们身体的免疫防御系统抵抗癌症侵袭,但抵抗癌症必须是长期且持续的。”加州大学洛杉矶分校血液学和肿瘤学教授Ribas说。“我们首次了解了肿瘤细胞可以避免被免疫系统T细胞识别,这样就降低了免疫系统对肿瘤细胞攻击的敏感性。”研究人员
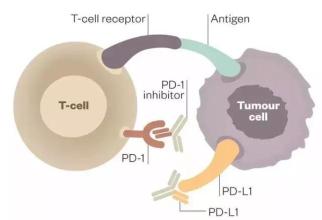
近日,加州大学洛杉矶分校研究人员发现一种机制,该机制确定了晚期黑色素瘤是如何对免疫检查点抑制剂进行抵抗的,这一发现可能会引起设计新型治疗方案来治疗致命的皮肤癌。
“免疫疗法可让我们身体的免疫防御系统抵抗癌症侵袭,但抵抗癌症必须是长期且持续的。”加州大学洛杉矶分校血液学和肿瘤学教授Ribas说。“我们首次了解了肿瘤细胞可以避免被免疫系统T细胞识别,这样就降低了免疫系统对肿瘤细胞攻击的敏感性。”
研究人员分析了接受单抗治疗的黑色素瘤病人的肿瘤活检组织。他们对病人开始治疗前和疾病复发后的肿瘤组织进行了对比。
在四组活检组织研究中研究小组发现了在一组肿瘤组织中丢失了一种称为B2M的肿瘤基因,该基因可被免疫系统识别。另外两组肿瘤组织的缺陷是可中断JAK1和JAK2基因的功能,这样就限制了免疫系统有效的杀死癌细胞。
“我们发现当免疫系统的T细胞非常活跃的时候,JAK1和JAK2产生的新改变可导致肿瘤对它们发送的信号(癌细胞停止增长)“选择性失聪”,而B2M基因的改变可降低免疫系统识别肿瘤的能力,这些发现可以帮助研究人员打开一个全新的研究领域,促使我们能够更好地理解这些治疗方法。”Zaretsky说。
研究人员还发现了第四组活检组织没有这些基因变异,这表明逃避免疫疗法的其它机制可能会在未来被发现,Zaretsky说。
原始出处
Jesse M. Zaretsky, B.S.et.al.Mutations Associated with Acquired Resistance to PD-1 Blockade in Melanoma.NEJM.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#阻断#
25
#色素#
30
#黑色素#
28
#黑色素#
21
厉害啊
80